
2023-2028 Texas State
Health Plan
As Required by
Texas Health and Safety Code
Section 104.021-104.026
Statewide Health Coordinating
Council
November 2022
This report was prepared at the direction of the Statewide Health
Coordinating Council. The opinions and recommendations
expressed in this report are that of the Council and do not reflect
the views of the Texas Health and Human Services Commission,
Department of State Health Services, or Texas Health and Human
Services System
2
Table of Contents
Table of Contents ................................................................................... 2
1. Executive Summary ........................................................................... 4
2. Background ....................................................................................... 6
3. Access to Care ................................................................................... 7
Defining Access to Care ....................................................................... 7
Populations with Poor Access ................................................................ 9
Texas Populations with Poor Access ................................................. 10
COVID-19 and Access ........................................................................ 13
Nationwide Access ........................................................................ 13
Access in Texas ............................................................................ 14
Race & Ethnicity ........................................................................... 14
Strategies for Improving Access .......................................................... 14
Covering More Texans ................................................................... 15
Provider Participation in Medicaid .................................................... 16
Other Policy Considerations ............................................................ 17
Policy Developments ..................................................................... 17
Policy Recommendations for the Legislature, the Governor, and Executive
Branch Agencies ........................................................................... 18
4. Rural Health .................................................................................... 23
Health Outcomes in Rural Areas .......................................................... 23
COVID-19 ................................................................................... 23
Emergency Medical Services ........................................................... 24
Teleservices................................................................................. 24
Older Adults in Rural Areas ............................................................ 24
Challenges for Low-Income and Uninsured Populations in Rural Areas ... 25
Hospital and Nursing Facility Closures .................................................. 25
Providers ......................................................................................... 26
Older Providers ............................................................................ 27
Obstetric Services......................................................................... 27
Policy Recommendations for the Legislature, the Governor, and Executive
Branch Agencies ........................................................................... 27
5. Mental Health and Behavioral Health Workforce ............................. 31
Background ..................................................................................... 31
Texas’ Need for Mental Health Services ................................................ 34
Children ...................................................................................... 34
Adolescents ................................................................................. 34
Adults ......................................................................................... 35
Texas’ Mental Health Workforce .......................................................... 36
3
Mental Health Workforce by Profession Among Racial/Ethnic Categories,
Texas, 2019 ............................................................................ 36
Overview of Mental Health Workforce by Profession ........................... 37
Policy Recommendations for the Legislature, the Governor, and Executive
Branch Agencies ........................................................................... 45
6. Teleservices and Technology ........................................................... 53
Defining Teleservices ......................................................................... 53
Use of Teleservices in Texas ............................................................... 53
COVID-19 and the Expansion of Teleservices ......................................... 54
Benefits of Teleservices ...................................................................... 55
Access to Teleservices ....................................................................... 56
Access in Rural Counties ................................................................ 56
Providers’ Ability to Deliver Teleservices ........................................... 56
Teleservices Post-COVID-19 ............................................................... 57
Policy Recommendations for the Legislature, the Governor, and Executive
Branch Agencies ........................................................................... 58
7. List of Acronyms .............................................................................. 60
Appendix A. Statewide Health Coordinating Council Roster ................. 62
8. References ...................................................................................... 64

4
1. Executive Summary
By November 1 of even-numbered years, the Statewide Health Coordinating Council
(SHCC) directs and approves the development of the Texas State Health Plan or its
updates for submission to the Governor. This plan, following the legislatively
determined purpose of the SHCC,
a
seeks to ensure that the state of Texas
implements appropriate health-planning activities and that health care services are
provided in a cost-effective manner throughout the state.
This State Health Plan focuses on how different factors affect health equity in the
state of Texas. The plan contains four sections that examine which groups are more
likely to have poorer access to care. The sections look at the challenges faced by
individuals residing in rural areas of the state, mental and behavioral health and the
ability of the state’s behavioral health care workforce to address these issues, and
finally, the role that teleservices can play in addressing health disparities.
Additionally, each section considers how COVID-19 has impacted health care in
Texas.
Based on the evidence contained within each chapter, the SHCC makes policy
recommendations consistent with goals of improving health care services in the
state and ensuring those services are cost-effective for Texans. These
recommendations include:
● Access to Care:
The state should support efforts to increase enrollment in Medicaid among
those that are eligible.
The state should examine the varied causes that limit access to care for
Texans.
● Rural Health:
The state should support new and innovative ways to bring health care
providers to rural areas.
The state should support new and innovative methods of hospital
financing.
a
See Texas Health and Safety Code Chapter 104 and Chapter 105.
5
● Mental Health and Behavioral Health Care Workforce:
The state should support efforts by schools to increase access to mental
health services for students.
The state should continue to support the work of the Texas Child Mental
Health Care Consortium.
The state should support efforts to increase the funding and stipends
available to students of the mental health professions as they complete
their education and training, as well as support the expansion of the Loan
Repayment Program for Mental Health Professionals.
● Teleservices and Technology:
The state should support new and innovative ways to get teleservices to
rural communities.
The state should encourage state, federal, and private health insurance
organizations to promote their teleservice benefits.
6
2. Background
With an eye toward improving access and health care delivery systems throughout
Texas, the 2023-2028 Texas State Health Plan provides guidance on how to achieve
a high-quality, efficient health system that serves the needs of all Texans.
Specifically, the plan identifies challenges in ensuring that a population as large and
diverse as Texas’ has access to the health care system, that health care services
are provided in an efficient and orderly manner, and that an ample health care
workforce exists to provide these services.
The plan is divided into four sections, each examining health challenges faced by
Texas and its health care workforce and proposing solutions to these challenges.
The first section focuses on issues related to differences in access to care for
individuals across the state. The second section places focus on unique health care
issues faced by those who live in rural Texas. The third section examines mental
health and behavioral health issues as well as ways to bolster the health care
workers in this field. The final section examines the impact of teleservices and
technology on the health care field, as well as how teleservices and technology may
aid in improving access to care.
7
3. Access to Care
This section discusses the health outcomes, health disparities, and demographic
differences among the Texas population. Additionally, the unique challenges faced
due to COVID-19 are discussed.
Defining Access to Care
Throughout much of Texas and the nation, access to health care is restricted by the
availability of providers, resulting in federal designations of health professional
shortage areas (HPSAs). This definition of access relies on the idea that those who
need health care can access the system if there is an adequate supply of services,
measured by the number of physicians, hospital beds, or some other metric.
1
Yet
these geographic designations do not fully reflect the multifaceted concept of
access to care. The Institute of Medicine has proposed the definition of access as
“timely use of personal health care services to achieve the best possible
outcomes”.
2
In addition to the availability of providers, this definition adds
components of timeliness and quality, the latter in the form of positive outcomes.
Another proposed definition of access is “fair access to consistently high quality,
prompt and accessible services right across the country”,
1
introducing the important
consideration of equity. This consideration is important given estimates that 30
percent of direct medical expenditures can be attributed to health disparities that
create a sicker population and that these disparities are associated with barriers to
accessing care.
3
The successful performance of health care systems at local, state, and national
levels is shown through the ability of individuals to access care when needed.
4
Simplistically, access may be considered the ease with which consumers and
communities are able to use appropriate services in proportion to their needs.
Access can then be considered in economic or other terms, such as the time
required to utilize health care services, travel distance to services, familiarity with
the health system and providers, and other considerations.
1,2,4
Researchers
4,5
have
proposed similar schema for categorizing potential barriers to access. Synthesized,
they are as follows:
• Affordability – Affordability refers to the ability of the patient to pay the
economic costs associated with health care. This may refer to directly
8
incurred costs or those associated with insurance coverage, including
premiums, deductibles, etc.
• Availability – Availability refers to the level of fit between the patient’s health
care needs and the ability of the system to fit these needs. For example,
availability is a measure of the nearness and capacity of clinicians and clinical
facilities.
• Acceptability – Acceptability refers to the ability of patients to interact with
the health care system in light of social, cultural, linguistic, and other norms
that may impede utilization.
• Appropriateness – Appropriateness refers to the extent to which the services
available fit the needs of the client. On the one hand, appropriateness may
refer to the patient’s level of comfort with the organization of the health
system, such as procedures necessary to garner an appointment, available
office hours, etc. On the other hand, this category may also include care
meeting the patient’s expectations with respect to elements such as
timeliness, the amount of time spent developing a diagnosis and treatment
plan, and the technical and interpersonal quality of the services rendered.
• Approachability – Finally, approachability refers to the extent to which
patients with health care needs are able to identify the appropriate services
available, are aware of how to reach them, and recognize the potential
impact on their health.
Of note, only one of the categories listed above is related to financial capacity of
the individual to pay for health care. While financial barriers to access are important
and associated with the presence of non-financial barriers, it is worthwhile to note
that of those reporting barriers to care, 66.8 percent of U.S. adults reported non-
financial barriers to care, a rate higher than those reporting financial barriers.
4
Seventy one percent of Medicaid patients and 49 percent of Medicare patients
reported non-financial barriers to accessing care.
With respect to availability, one of the main barriers to access that exists is a lack
of specialists and subspecialists in low-income and rural areas. For example, one
survey found that 91 percent of community health centers struggled to find
adequate off-site subspecialty care for their uninsured patients.
6
A major concern regarding acceptability is the extent to which patients are able to
receive information and instructions in their preferred language. Often linguistically
9
based barriers can result in the delay or even denial of services, challenges with
medication management, and the underutilization of preventive services.
7
The
National Committee for Quality Assurance and the Joint Commission on the
Accreditation of Healthcare Organizations are beginning to recognize the role that
language services play in the provision of quality health care. Clinical staff may
need training on when to request a medical interpreter, as unqualified interpreters
may lead to medical errors and poor patient understanding and adherence.
With respect to appropriateness, research
2
has noted that patients often experience
a cumulative burden of barriers and are frequently in need of multiple avenues
through which to access care. For example, offices seeking to increase
appropriateness might work to reduce wait times for appointments, alter their office
hours to reflect the needs of their clients, and offer advice by phone where
appropriate: all key components of the patient-centered medical home. Research
on community health centers, which often serve populations with low access, show
greater patient satisfaction not only with hours of operation but with overall care.
Finally, approachability relies on the patient to recognize when they are in need of
health services and to utilize these services, a term referred to as patient
activation.
8
Of note, different rural populations may require different strategies for
ensuring patient activation, and rural populations are likely to require different
strategies than metropolitan areas.
4,8
Ultimately, access to healthcare is a complex
idea that can be understood through all of the definitions provided.
Populations with Poor Access
In all, 18 percent of US adults experienced financial access barriers and 21 percent
experienced non-financial barriers.
5
Such barriers have been growing in the past
decade, resulting in decreased likelihood of adults having a usual source of care,
having recently seen a dentist, and having recently had a medical office visit.
9
Generally, poor access is higher in lower-income, non-white, and young adult
populations, in addition to individuals with at least one chronic disease.
5,10
Some of
these access challenges are related to affordability as racial and ethnic minorities
often comprise a disproportionate percent of the uninsured, despite absolute and
relative improvements in the rates of insurance coverage of Hispanics and African
Americans.
10,11
Indeed, reports show that access to care declined in all adult
populations from 2000 to 2010 with the most dramatic declines present in
uninsured populations.
9
Thus, it comes as no surprise that being uninsured is
associated with foregoing needed care because of cost, not having a usual source of
care, not receiving recommended screening activities, high-risk adults not getting
10
checkups in the past two years, and patients with diabetes not receiving
recommended diabetes care.
12
According to the Institute of Medicine
13
, uninsured pregnant women receive fewer
prenatal care services than insured pregnant women and are more likely to have
poor birth outcomes, including low birthweight and prematurity. Following
pregnancy, women need ongoing care for both physical and behavioral health
needs, including treatment for chronic conditions such as diabetes and
hypertension, as well as diagnosis and treatment for postpartum depression and
substance use disorders. Women without health insurance often lack access to
affordable contraceptives, including the most effective forms known as Long-Acting
Reversible Contraceptives, which includes intrauterine devices and implants.
Without access to contraceptives women are more likely to experience unintended
pregnancies. Further, uninsured women with breast cancer are 30–50 percent more
likely to die from cancer or cancer complications than insured women with breast
cancer. Uninsured women are 60 percent more likely to receive a diagnosis of late-
stage cervical cancer.
13
Additionally, considerably more Hispanic and multiracial families reported needing
an interpreter than white families.
11
These barriers may partially explain why lower
proportions of Hispanics, African Americans, and multiracial children receive needed
medical and dental care and why access to specialty care is worse for Hispanics and
African Americans.
Texas Populations with Poor Access
Women and Men
Women and men in Texas have unique issues that affect access to health care
services. When compared to men, women have similar rates of health insurance by
type with 62.3 percent carrying private insurance, 17.3 percent with
Medicaid/Children’s Health Insurance Program (CHIP), and 16.8 percent
uninsured.
14
The percentages of men who are uninsured are similar, with 18.4
percent uninsured. Texas men are less likely to have a personal doctor when
compared to women, with 28.9 percent of women and 37.6 percent of men
reporting not having at least one personal doctor or health care provider.
15
On the
other hand, women have reported higher rates of not being able to access medical
care due to costs, 17.2 percent compared to 13.0 percent of men.
When considering geographic distribution, men and women in border areas have
higher rates of uninsuredness than those in non-border areas.
16
While 24.5 percent
11
of both men and women in the state of Texas report not having health care
coverage, 37.9 percent of those living in border areas report not having coverage.
Furthermore, uninsuredness is higher for women than men in non-border areas,
with 42.0 percent of women reporting that they do not have coverage, while 33.8
percent of men reported that they do not have coverage.
Low-Income and Less Educated Populations
Health care access for low-income Texans varies based on socioeconomic position.
Over 44 percent of Texans at or below the federal poverty line (FPL) rely on
Medicaid as their primary insurance, while 23.7 percent rely on private insurance.
16
Almost 30 percent of Texans living at or below the FPL are uninsured. Use of
Medicaid is less common as socioeconomic position rises, dropping to 27.2 percent
for families whose income is at 200 percent of the FPL or below. Table 1 shows the
percent of Texans who are uninsured and the percent of Texans that do not have a
personal doctor separated by income.
Table 1. The percent of Texans that are uninsured and do not have a personal
doctor by income level
15
Annual Income Percent Uninsured
Percent that do not have a
Personal Doctor
<$25,000 52% 45.7%
$25,000-$49,999 25.6% 34.5%
$50,000-$74,999 20.9% 24.2%
b
$75,000-$99,999 16%
$100,000+ 8.7%
The percentage of Texans that are uninsured continues to drop as annual income
increases and lower income Texans are more likely not to have a personal doctor.
Insurance coverage is more likely among higher educated groups.
16
For example,
among those aged 25+ years with less than a high school education, 38.8 percent
b
24.2% of Texans with an annual income of $50,000 or more do not have a personal
doctor.
12
reported being uninsured. By comparison, 24.6 percent of high school graduates,
15.7 percent of those with some college, and 7.9 percent of college graduates
reported being uninsured. Likewise, 22.1 percent of those without a high school
degree reported having been unable to see a doctor when they needed to because
of cost.
15
For high school graduates, the percentage was 15.0 percent. For those
with some college and college graduates, the percentages were 16.3 percent and
9.8 percent respectively.
Children
Eleven percent of Texas children, 854,340 individuals, do not have health
insurance.
16
For those with health insurance coverage, 53.2 percent use private
health insurance and 37.9 percent are enrolled in Medicaid/CHIP. Children that
reside in households that earn 300 percent of the FPL or below have uninsured
rates between 12 and 17 percent while those above 300 percent of the FPL have
uninsured rates of 6 percent.
15
Adult Populations
Texans between the ages of 19 to 44 are uninsured at rates that fall between 25.1
and 30.2 percent.
16
For Texans that fall in the 45 to 54 year age group, only 20.6
percent reported having no health insurance coverage. For those 65 years of age or
older, only 1.8 percent reported no health insurance coverage. Over half of younger
Texans ages 18 to 29 do not have a personal doctor compared to 43.7 percent for
those ages 30 to 44, 24.7 percent for those 45-64, and 9.1 percent for those ages
65+. Between 16.5 and 19.1 percent of Texans aged 18 to 64 reported that they
were unable to see a physician due to costs. Only 5.3 percent of those aged 65+
were unable to see a physician due to costs.
15
Minority Groups
Hispanics in the state of Texas have significantly higher rates of being uninsured
when compared to other racial groups. The percentage of Hispanics that do not
have health insurance coverage is 27.3, compared to 10.0 percent of whites, 15.0
percent of African Americans, and 11.4 percent from other racial backgrounds.
16
White and African American Texans are more likely to have a personal doctor (75.6
percent of whites and 76.4 percent of African Americans), when compared to
Hispanics at 52.9 percent. Percentages of Hispanics and African Americans that
were unable to access a physician due to costs were similar, at 20.2 and 14.7
percent respectively, while only 11.3 percent of whites and 12.2 percent of multi-
racial or other-raced individuals were unable to see a physician due to costs.
15

13
Border Counties
c
Texans that reside near the Texas/Mexico border are less likely to have health
insurance coverage when compared to the state as a whole, 37.9 percent compared
to 24.5 percent.
16
When considering only those aged 18-64 in non-border areas of
the state, those who were uninsured was estimated to be 21.9 percent. In border
areas, this percentage was almost doubled at 38.5 percent. The border region also
has higher rates of Medicaid utilization when compared to the rest of Texas, 27.3
percent compared to 16.2 percent. Additionally, those living in border areas are less
likely to have a personal health care provider, more likely to forgo needed medical
treatment because of cost, and less likely to have had a routine checkup in the past
year.
15
COVID-19 and Access
Nationwide Access
Communities across the U.S. and specifically in Texas have been impacted by
COVID-19, with communities being impacted in different ways.
17
Due to the high
demands of COVID-19 on medical staff, many individuals have reported
experiencing reduced access.
18
This issue was particularly severe in the earlier
months of the pandemic. According to experimental survey research, in June and
July of 2020, 38.7 percent of adults reported that they were unable to receive one
or more types of care in the past two months due to the pandemic. This percentage
dropped to 28.2 percent in August 2020. In May and June 2021, it had fallen
further to 12.7 percent. According to the study, in each time period, women were
more likely than men to report that the pandemic had caused them to be unable to
receive one or more types of medical care.
18
Furthermore, the onset of COVID-19
resulted in 5.4 million lost jobs in the U.S. and for many Americans the loss of a job
also resulted in the loss of health insurance, reducing millions’ access to health
care.
19
c
Border area is defined through the La Paz Agreement of 1986 and includes 32 Texas
Border counties: Brewster, Brooks, Cameron, Crockett, Culberson, Dimmit, Duval, Edwards,
El Paso, Frio, Hidalgo, Hudspeth, Jeff Davis, Jim Hogg, Kenedy, Kinney, La Salle, Maverick,
McMullen, Pecos, Presidio, Real, Reeves, Starr, Sutton, Terrell, Uvalde, Val Verde, Webb,
Willacy, Zapata, and Zavala.
14
Access in Texas
According to one study, an estimated 659,000 Texans lost health insurance as a
consequence of job-loss due to COVID. Another study suggests the number of jobs
lost may be even higher, indicating that as many as 1.6 million Texans lost their
employer-sponsored health insurance due to job-loss during the COVID-19
pandemic.
20
Such losses during the pandemic are particularly concerning because
when individuals are without health coverage they tend to delay seeking medical
attention.
19
This may have led to additional spread in the virus among those who
did not know that they were infected.
Race & Ethnicity
Additional concerns around COVID-19 relate to differences in vaccination rates
based on race. One major concern, particularly early in the vaccination distribution
process, was ensuring that communities had equal access to the vaccine.
21
As of
2022, in Texas, 53 percent of white individuals have received at least one dose of
the vaccine, while only 46 percent of African-American individuals have been
vaccinated. In contrast, 59 percent of Hispanic individuals have been vaccinated,
and 73 percent of Asian individuals have been vaccinated in Texas.
22
Nationally, 48
percent of white individuals, 32 percent of African-American individuals, 27 percent
of Hispanic individuals, and 48 percent of Asian individuals have received at least
one dose of the vaccine.
23
Texas exceeds vaccination rates among race/ethnicity
categories compared to the nation as a whole.
Strategies for Improving Access
Three broad strategies are available to address the gaps in access to care identified
above: improving rates of insurance coverage; increasing the availability of health
care professionals, facilities, and services; and a reduction in social barriers to care.
Ultimately, improving timely access to and quality of care will depend on
collaboration among local clinicians, hospital leaders, insurance companies,
policymakers, and community stakeholders.
12
Success in improving access to care
relies on concurrent efforts to reduce financial and nonfinancial access barriers.
5
Additionally, Texas has fewer physicians per capita than the national average,
creating additional hurdles for those who need access to care.
24
Increasing the
number of available physicians and other health care providers will improve access
and lessen the burden on those health care professionals in the state. A
fundamental aim of the redesign of primary care services is improving access to
care. Patients who reported having a usual site of care and a provider at that site
15
are more likely to access that care, receive preventive services, and have improved
health.
2
The following strategies seek to improve access by making health care
more affordable, available, acceptable, appropriate, and approachable.
Covering More Texans
In order to improve the affordability of care and thus access in Texas, it should be a
priority of this state to increase the number of Texans with insurance coverage and
a usual source of care. This can be accomplished through greater public coverage of
the poor and improved access to physicians and other providers within the public
system. Projections
25
demonstrated that low-income Medicaid enrollees were
significantly more likely to have a usual source of care and less likely to have
unmet health care needs. Publicly covered adults are also more likely to report
timely care and less likely to delay or go without needed medical care because of
costs.
With respect to mothers and their children, increasing the percentage of covered
mothers is likely to have a significant effect on access to health care, ability to pay
medical bills, and mental health. Children are also expected to benefit, since their
coverage and access to care have been shown to improve when their parents have
coverage. Increasing the number of mothers with insurance may also improve
outcomes for children in other ways, such as by reducing maternal depression,
which can affect parenting abilities.
Medicaid, along with its companion CHIP, is a state/federal partnership that
provides health care coverage to low-income children and their caretakers,
pregnant women, people age 65+, and people with disabilities. Some states,
though not Texas, have chosen to extend Medicaid coverage to childless,
nondisabled, working age adults.
In Texas, the Medicaid and CHIP programs cover over four million people.
26
A large
body of evidence suggests that these individuals are more likely to have a usual
source of care, more likely to receive preventive health services, and less likely to
have unmet or delayed needs for medical care than if they were uninsured.
25
Research has consistently indicated that people with Medicaid coverage fare much
better than their uninsured counterparts on measures of access to care, utilization,
and unmet needs. Evidence further shows that, compared to low-income uninsured
children, children enrolled in Medicaid are significantly more likely to have a usual
source of care and to receive well-child visits and immunizations, and significantly
less likely to have unmet or delayed needs for medical care, dental care, and
prescription drugs due to costs. Moreover, in some states that expanded Medicaid,
16
reports note that the expansion led to improvements in prenatal care use, in terms
of either earlier or more adequate prenatal care.
The federal government currently subsidizes, via tax credit, marketplace health
insurance premiums for households that earn from 100 percent to 400 percent of
the FPL.
13
Texas adults earning below the FPL, but who do not qualify for Medicaid
or for federal subsidies to purchase care on the insurance exchange, fall into what
is known as the “coverage gap.” Nationally, over two million poor uninsured adults
fall into the coverage gap, a third of which reside in Texas. In total, there are
771,000 people that fall into the coverage gap in Texas, leaving them with no
realistic options for affordable health insurance coverage.
Provider Participation in Medicaid
In order to improve access to care in Texas, it is important to address shortages in
providers treating low-income individuals. Among the challenges providers face are
the administrative burden of participation in Medicaid, the complexity of many
patients’ needs, challenges in arranging mental health and specialty referrals, large
patient panels associated with a general shortage of physicians, and lower
reimbursement rates than other payers. National research has indicated that
physicians may be optimistic about the ability of electronic health records and
medical homes to mitigate challenges.
27
With respect to reimbursement, Texas is one of 22 states that pays 75 percent or
less for Medicaid physician fees when compared to Medicare physician fees.
5
There
are 24 states that pay physician fees at 75 percent to 100 percent and three that
pay greater than 100 percent for services under state-run Medicaid programs when
compared to Medicare. Texas Medicaid pays approximately 65 percent compared to
the federally funded Medicare program.
3
Due to the gap in physician reimbursement
between the two programs, physician participation has diminished. The number of
Texas physicians willing to accept new Medicaid patients fell from 67 percent in
2000 to 31 percent in 2012
4
and increased slightly to 34 percent in 2015.
1,3
In
order to guarantee strong provider networks for Texas low-income residents, Texas
should strive to pursue a comprehensive approach to improving provider experience
and increasing participation in Medicaid.
From 2013 to 2014, the federal government provided additional funding that
allowed states to increase Medicaid payments to primary care physicians to match
payments for the same services through Medicare.
28
These funds successfully
sought to increase participation in Medicaid programs, especially primary care
17
services, effecting a five percent rise in physician participation in Medicaid during
this time.
1,3
However, the increase in payments was not made permanent in Texas.
Other Policy Considerations
Generally, the racial and ethnic profile of health care providers in Texas does not
reflect that of the population at-large. In addition to cultural preferences pondered
in the mental health section of this report, it has been shown that minority
physicians are significantly more likely to care for minorities, the publicly insured,
and uninsured patients.
11
Likewise, a more diverse workforce may help address the
need for linguistic competency within the health provider workforce. In the interim
though, the standardization of payment mechanisms for interpreter services and
their inclusion in health plans may improve access for those who are not proficient
in English.
7
The expansion of teleservices, the appropriate utilization of physician assistants and
advanced practice registered nurses, and stronger financial incentives for clinicians
to practice in underserved areas may be useful for expanding access in
geographically underserved areas.
5
Policy Developments
The Delivery System Reform Incentive Payment (DSRIP) pool in the Texas
Healthcare Transformation and Quality Improvement Program Medicaid 1115
Demonstration (Waiver) began in 2012 and was set to conclude in September
2021.
29
The DSRIP program benefitted Texans and the Texas health care delivery
system. Texas providers earned over $15 billion in DSRIP funds from 2012 to
January 2019, and it served 11.7 million people and provided 29.4 million
encounters from October 1, 2013 to September 30, 2017. As the DSRIP pool came
to a close, the state of Texas began working on new programs to support services
in Texas. As part of the DSRIP transition plan, several programs that offer access to
care, often for underserved communities, have been introduced. The Health and
Human Services Commission (HHSC) submitted the following programs, which have
been approved:
● Texas Incentives for Physician and Professional Service (TIPPS)
30
: A value-
based directed payment program for certain physician groups providing
health care services to children and adults enrolled in the STAR, STAR+PLUS
18
and STAR Kids Medicaid programs.
d
Eligible physician groups include health-
related institutions, indirect medical education physician groups affiliated
with hospitals, and other physician groups.
● Comprehensive Hospital Increased Reimbursement Programs
31
: A directed
payment program for hospitals providing health care services to adults and
children enrolled in STAR and STAR+PLUS. Eligible hospitals include
children's hospitals, rural hospitals, mental health hospitals, state-owned
hospitals, and urban hospitals.
● Directed Payment Program for Behavioral Health Services
32
: A directed
payment program for community mental health centers to promote and
improve access to behavioral health services, care coordination, and
successful care transitions. It also incentivizes continuation of care for STAR,
STAR+PLUS, and STAR Kids members using the Certified Community
Behavioral Health Clinic model of care.
● Rural Access to Primary and Preventive Services
33
: A directed payment
program for rural health clinics that provide primary and preventative care
services to STAR, STAR+PLUS, and STAR Kids members.
Policy Recommendations for the Legislature,
the Governor, and Executive Branch Agencies
Encourage the use of health care teams that include different types of
health care providers.
In 2021, 34 of the 254 counties in Texas had no primary care physicians and 31
counties had no direct patient care physicians.
24
Using teams that include different
types of health care providers can facilitate the provision of care for those without
physicians nearby. Using teams also promotes more efficient care in addressing the
health care needs of patients and provides physicians with the opportunity to focus
on the more serious and complex needs of patients. This shift would help to
redistribute responsibilities and allow physicians to utilize their time working with
those patients who need their expertise. This would allow physicians to more
efficiently allocate their time, which is critical due to the shortage of physicians in
the state.
d
STAR, STAR+PLUS, and STAR Kids are Texas Medicaid and CHIP Programs. More
information about the individual programs can be found at
https://www.hhs.texas.gov/services/health/medicaid-chip/medicaid-chip-members
.
19
Conduct a study examining which factors decrease physician participation
in Medicaid programs.
Improving our understanding regarding why more physicians do not participate in
Medicaid is an important first step in increasing access. Many factors may influence
physicians’ decision to not participate in Medicaid programs, such as the process of
becoming a Medicaid provider, patient participation, reimbursement rates, etc.
Understanding the hurdles preventing physicians from participating will allow for
more targeted approaches in improving physician participation in Medicaid which
would improve access for many Texans.
Support the furthering of health literacy and utilization of preventative
services for those on Medicaid.
According to the CDC, health literacy is “the degree to which individuals have the
ability to find, understand, and use information and services to inform health-
related decisions and actions for themselves and others.”
34
Furthering health
literacy would aid in improving health outcomes.
35
Research has shown that
patients who are better informed make better choices for their health, ultimately
improving health outcomes. Health literacy is also key for effective preventative
medicine.
36
Health literacy helps prevent health problems, protect individuals’
health, helps people better manage health problems when they arise, and improves
individuals’ ability to identify health problems early, which is often key to
treatment.
37
Additionally, preventative medicine improves health outcomes, and
increasing the utilization of such services would improve the health of Texans.
38
During the 87
th
Legislature, Regular Session, the House Select Committee on Health
Care Reform was created. The committee’s duties are to “examine the potential
impact of delayed care on the state’s health care delivery system, health care costs,
and patient health outcomes, as well as best practices for getting patients with
foregone or delayed health interventions back into the health care system. The
study should consider patient delays in obtaining preventative and primary health
services…” Together, improving health literacy and utilization of preventative
services for those on Medicaid could improve the health of Texans across the state.
Support efforts to increase enrollment in Medicaid among those that are
eligible.
During the 87
th
Legislature, Regular Session, the House Select Committee on Health
Care Reform was created. The committee is charged with studying ways to improve
20
outreach to families with children who are eligible for, but are not enrolled in,
Medicaid or CHIP. This targets increasing enrollment of children who are eligible,
but there should also be similar efforts to increase outreach for all those who are
eligible for Medicaid but not enrolled in the program.
Continue to support programs like TIPPS, which provides increased
Medicaid payments to certain physician groups providing health care
services to persons enrolled in STAR, STAR+PLUS, and STAR Kids.
On March 25
th
, 2022 the TIPPS program was approved by the Centers for Medicare
and Medicaid Services.
32
This program is for delivery system and provider payment
initiatives under Medicaid managed care plan contracts. Three classes of providers
are eligible to participate: (1) health-related institution physician groups, (2)
physician groups affiliated with hospitals that receive indirect medical education
funding, and (3) other physician groups.
TIPPS funds are paid through three components of the managed care capitation
rates:
• Component 1 is equal to 65 percent of the total program value and provides
a uniform dollar increase paid monthly. Only health-related institutions and
indirect medical education physician groups are eligible for Component 1.
• Component 2 is equal to 25 percent of the total program value and provides
a uniform rate increase paid semi-annually. Only health-related institutions
and indirect medical education physician groups are eligible for Component 2.
• Component 3 is equal to 10 percent of the total program value and provides
a uniform rate increase for applicable outpatient services and is paid at the
time of claim adjudication. All participating physician groups are eligible for
Component 3.
Increased Medicaid payments compensate providers and may encourage greater
participation in the programs, which would increase the capacity to provide care to
those on Medicaid.
Support the development of quality thresholds that must be met by those
providers participating in TIPPS.
The TIPPS program has the following quality goals:
21
• Promote optimal health for Texans at every stage of life through prevention
and by engaging individuals, families, communities, and the health care
system to address root causes of poor health.
• Promote effective practices for people with chronic, complex, and serious
conditions to improve people’s quality of life and independence, reduce
mortality rates, and better manage the leading drivers of health care costs.
Subsequently, TIPPS providers must provide qualitative and numeric data, which
will be used to monitor provider-level progress toward state quality objectives.
While these quality measures must be reported, there are no minimums that
currently must be met so there should be a shift to developing standards that would
assess whether care is meeting or exceeding the quality goals that have been
developed.
Examine the varied causes that limit access to care for Texans.
While affordability plays a role in access to care, it is only one factor to consider
when examining barriers to health care. Lawmakers should further examine other
factors that limit access to care. This includes the level of fit between patients’
health care needs and the ability of the system to fit these needs, which includes
the nearness and capacity of clinicians and clinical facilities.
5
Another factor that
should be examined is the ability of patients to interact with the health care system
in light of social, cultural, linguistic, and other norms that may impede utilization.
These factors are particularly important due to the large Hispanic population in the
state. Texas had a higher percentage of individuals five years of age and over who
spoke a language other than English at home (35.5 percent) compared to the
nation (21.5 percent) from 2014 to 2018.
39
Texas has the second highest
percentage of individuals who spoke a language other than English at home (behind
California). The most common language other than English spoken at home in
Texas was Spanish (29.5 percent), followed by Asian and Pacific Islander languages
(2.9 percent) and other Indo-European languages (2.2 percent).
Additionally, the extent to which the services available fit the needs of the patient
should also be examined.
5
This may include the patient’s level of comfort with the
organization of the health system. It may also include care meeting the patient’s
expectations with respect to elements such as timeliness, the amount of time spent
developing a diagnosis and treatment plan, and the technical and interpersonal
quality of the services rendered. Finally, the extent to which people with health care
needs are able to identify the appropriate services available, are aware of how to
22
reach them, and recognize the potential impact on their health should be included
when examining access to care.
23
4. Rural Health
This section discusses the health outcomes, health disparities, and demographic
differences in rural areas throughout the state of Texas. Additionally, the unique
challenges faced by hospitals and health practices are discussed.
Health Outcomes in Rural Areas
Nationally, residents in rural areas have a life expectancy 1 to 5 years less than
residents in urban areas.
40
Those in rural areas are more likely to smoke, less likely
to exercise, and have less nutritional diets than those in suburban areas.
41
These
factors contribute to higher mortality rates and higher rates of chronic diseases in
rural areas. Approximately 43 percent of deaths in rural areas can be attributed to
modifiable risk factors such as smoking, excessive drinking, and obesity, compared
to about 37 percent in urban areas.
42
Rural residents are more likely to have
hypertension, diabetes, arthritis, and high cholesterol than urban residents. Rural
children are more likely to be obese than urban children.
43
Rural areas also have
higher age-adjusted mortality for heart disease, cancer, chronic respiratory disease,
and stroke.
44
In 2019, the age-adjusted mortality was 834.0 per 100,000
population in rural communities and 693.4 in urban communities.
45
Rural residents
were also more likely to die due to unintentional injury, drug poisoning, and suicide
than urban residents.
Rural health in Texas faces both similar and unique challenges compared to rural
health nationally.
46
The rural populations of Texas are incredibly diverse; for
example, the Texas-Mexico border area is predominantly Hispanic (88.4 percent)
compared with the rest of the state (35.5 percent).
47
There are colonias, which are
“residential area[s] lacking some basic infrastructure like a drinking water supply,
sewage treatment, paved roads, adequate drainage, etc.”
48
Adult residents of
colonias report worse physical health compared to adults nationally and Hispanic
adults as a whole.
49
COVID-19
The first pandemic surge in Spring 2020 resulted in higher incidence and mortality
in urban areas. During the second surge in Summer 2020, the rates in rural areas
surpassed those in urban areas. Since then, incidence and mortality rates have
remained higher in rural than urban areas.
50
Rural areas felt a greater impact from
COVID-19 due to poor health literacy and health care infrastructure, as well as
24
having higher proportions of elderly and people with comorbidities.
51
Rural areas
have higher incidences of underlying medical conditions that increase the risk of
severe illness from COVID-19, such as obesity, diabetes, hypertension, and
smoking.
52
Rural areas also tend to have lower COVID-19 vaccination rates.
53
Residents of rural areas are more likely to distrust vaccines than those of urban
areas.
54
Emergency Medical Services
Emergency medical services (EMS) face challenges in rural Texas.
55
As
requirements for EMS personnel increase and access to training in rural Texas
decreases, this exacerbates staffing issues in rural Texas. Rural EMS providers tend
to be staffed less than urban EMS. EMS agencies are often staffed by volunteers or
a mix of volunteers and paid staff. One study found that those agencies staffed by
volunteers are often less trained and would benefit from additional training for their
positions.
56
Additionally, a study found that rural EMS are more likely to lose staff
to burnout than urban EMS. The closure of rural hospitals also puts strain on EMS
by increasing drive times to facilities.
57
The Texas Department of Transportation
Safety Division through the Texas A&M Engineering Extension Service provides
funding for Texas Rural/Frontier EMS training; however, funds are limited.
55
Senate
Bill 8 of the 87
th
Legislative Session, 3
rd
Special Session, allocated funding for EMS
education programs.
58
This included $21 million that goes towards scholarships for
EMS students with special consideration for those in rural parts of Texas.
59
Teleservices
The current COVID-19 pandemic has resulted in the rapid expansion of telehealth
and telemedicine services. The Centers for Medicare and Medicaid Services has
expanded the number of services eligible for telehealth.
60
Additionally, emergency
rules were issued expanding telehealth and telemedicine.
61
A report identified
telemedicine as a way for rural residents to access subspecialist services and for
expanding services offered by nurse practitioners and physician assistants.
62
Broadband access is a barrier to receiving telehealth and telemedicine in rural areas
of Texas.
55
There are over 2 million households in Texas without high-speed
internet access.
63
Fiber infrastructure and broadband access have been identified as
a key concern among rural residents.
55
Older Adults in Rural Areas
Nationally, the rural population is older than the urban population.
64
In 2015, the
median age was 51 years in rural areas and 45 in urban areas. Rural communities
25
also had a higher proportion of people aged 65 and older in 2016, as this age group
comprised 18.4 percent of the population in rural areas compared to 14.5 percent
in urban areas. According to the Texas Demographic Center, rural counties
experienced the greatest increases in median age from 2010 to 2018.
65
For
instance, 18 percent of rural counties saw an age increase of two to four years, and
16 percent saw an increase of more than four years. Metropolitan counties saw an
age increase of two to four years in 13 percent of counties and more than four
years in only 2 percent of counties. Older adults are at higher risk of chronic
disease, and many manage two or more chronic conditions.
66
Older adults often
require more complex health care that may be more difficult to receive in rural
areas.
Challenges for Low-Income and Uninsured Populations in
Rural Areas
In 2018, Texas had the highest number of uninsured people in any state.
67
Rural
households also report a lower median income than urban households.
64
In 2016,
the median income was $46,000 for rural households and $62,000 for urban
households. Moreover, the poverty rate was 16.9 percent in rural areas and 13.6
percent in urban areas. In 2013, the food insecurity rate was 15.8 percent in rural
communities and 14.5 percent in urban communities. Low-income communities
have limited access to fresh foods and environments that are conducive to physical
activity.
68
Income and poverty have been established as being associated with poor
health and increased mortality.
In summation, people that live in rural areas tend to have poorer health outcomes
when compared to their urban counterparts. These issues are highlighted by the
lower incomes and lower insurance rates in rural areas. These issues make rural
health access complex and highlight why the issues surrounding facilities and
providers, as discussed below, are particularly important.
Hospital and Nursing Facility Closures
Access to quality health services was identified as the top priority in rural health
over the last decade.
46
Types of access that were identified as the most concerning
include emergency services, primary care, and insurance. Since 2010, 26 rural
hospitals have closed in Texas.
69
Hospital closures in rural areas negatively impact
access to care and potentially health outcomes as well.
70
Hospital closures lead to
loss of access to emergency care, making emergency medical transport even more
important. For patients that rely on hospitals for specialty care or referrals, they
26
lose that access as well. In particular, communities often lose access to obstetric
care, mental health care, and diagnostic testing when hospitals close. Communities
that lose hospitals have a difficult time recruiting employers and industries to the
area.
Hospital closures can lead to increases in the amount of time patients must travel
to obtain care.
71
Longer travel times can lead to negative health outcomes,
especially for conditions like traumatic injuries and stroke.
There was a significant amount of nursing home closures between June 2015 and
June 2019.
72
Research shows there were 555 nursing home closures nationwide
during these years, including 65 in Texas. Moreover, 40 percent of the nursing
home closures in Texas were in rural areas.
In 2018, Texas had the highest number of uninsured people in any state, and Texas
has not expanded Medicaid through the Affordable Care Act (ACA).
67,73
People of
color are more likely to be low-income and uninsured, so Medicaid expansion
affects them more significantly.
75
Additionally, the ACA expansion of Medicaid has
been found to be associated with reduced probabilities of hospital closures.
76
In
states that expanded Medicaid, rural hospitals increased revenue that likely reduced
the number of closures.
Providers
Data from the Texas Department of State Health Services (DSHS) indicate that
non-metropolitan counties had 36.7 percent fewer primary care physicians per
capita than metropolitan counties in 2021.
24
Non-metropolitan counties had 56.6
percent fewer direct patient care physicians per capita than metropolitan counties.
In the same year, there were 34 counties in Texas with no primary care physicians
and 31 counties with no direct patient care physicians.
Some reasons why health care clinics close include physician retirement or because
they, like hospitals, are not financially solvent. Clinic closures in rural Texas can
lead to longer drives to access care and delaying care due to the distance.
77
An
example was highlighted in a news article that described the impact of the closure
of the clinic in Cottle County that resulted in one resident having to drive 30
minutes to Childress County, the next closest clinic. Residents in rural areas must
make hard choices about whether or not to move to obtain better access to care,
especially as they age.
27
Older Providers
As illustrated by data from DSHS, direct patient care physicians in rural Texas areas
tend to be older.
24
In 2021, the median age of direct patient care physicians was 49
years in metropolitan counties and 56 years in non-metropolitan counties.
As physicians in rural areas age and retire, they may leave practices that have to
close because there are no physicians in the area to continue the practice.
78
When
the nurse practitioner who ran the only health clinic in Memphis, Texas retired, the
clinic closed. Now residents must drive approximately 140 miles to receive care.
Obstetric Services
According to DSHS data, non-metropolitan counties had 63.4 percent fewer
obstetricians and gynecologists per capita than metropolitan counties in 2021.
24
Projections show that the shortage of obstetricians and gynecologists is projected to
continue through 2032 in seven of the eight public health regions in Texas.
79
Nationally, the number of hospitals providing obstetric care in rural areas has
decreased over the last 20 years.
80
This can lead to increased travel time for
women in rural areas. A study that examined factors associated with rural obstetric
unit closures found that common risk factors included: low number of births,
private hospital ownership, low number of family physicians in county, and lower
income county.
As obstetric units close, women must drive farther distances to give birth.
80
This
may be dangerous for women with high-risk pregnancies or complications. Obstetric
unit closures in rural counties that are not adjacent to urban counties are
associated with higher rates of preterm births.
81
Policy Recommendations for the Legislature,
the Governor, and Executive Branch Agencies
Support new and innovative methods of hospital financing.
Hospital financing is a significant factor in whether a hospital stays in a rural area.
By encouraging innovative financing, Texas can create novel solutions to strengthen
rural hospitals. In the report from Texas A&M University, facility conversion is
identified as a solution for hospitals.
62
Another model, the Pennsylvania Rural
Health Model, transitions rural hospitals from fee-for-service to global budget
28
payments.
82
The Texas A&M University Rural and Community Health Institute
provides technical assistance to rural hospitals in such areas as finance challenges,
grant writing, and community engagement.
83
By evaluating services, hospitals can best adjust their services to meet the needs of
the community. Additionally, facilities can formalize relationships with other
facilities to provide other services. Sharing resources such as key personnel, health
information technology, and board membership can help to optimize limited fiscal
resources and improve continuity of care.
84
Monitor the impact of the coronavirus pandemic on the number of
uninsured people in Texas.
Prior to the coronavirus pandemic, Texas had the highest number of uninsured
people of any state. More than 4.9 million people in Texas, or about 17.3 percent of
the state’s population, were uninsured in 2020.
85
An estimated 659,000 adults in
Texas lost coverage due to job loss during the pandemic.
86
As this is a rapidly
changing situation, leaders must continue to track and determine the impact of the
pandemic on the number of uninsured people in the state.
Monitor the impact of the coronavirus pandemic on the shortage and
maldistribution of health care providers.
A survey conducted by the American Association of Critical Care Nurses found that
92 percent of respondents felt that the pandemic had “depleted nurses at their
hospitals and, as a result, their careers will be shorter than they intended.”
87
Many
physicians are also experiencing burnout due to the pandemic.
88
Nationally,
employment in the health care field is down by 306,000, or 1.9 percent, since
February 2020.
89
This could exacerbate the existing workforce maldistribution in the
state and shortage in rural areas. Notably, the number of Texas counties
designated as primary care shortages areas jumped from 129 in 2019 to 228 in
2021.
90
During the pandemic, many nurses left their jobs to become traveling nurses due to
higher earning potential. The nursing shortage has driven up the price of traveling
nurses, making employing them much more costly to hospitals that are
experiencing staffing shortages.
91
To adequately provide for the medical needs of all
Texans, the state must correct its chronic shortage and maldistribution of health
care providers.
29
Support expanding the state’s loan repayment programs to include more
health professions.
The Texas Higher Education Coordinating Board has loan repayment programs for
physicians, nurses, and mental health professionals who practice in underserved
areas.
92
Two of these are the State Physician Education Loan Repayment and Rural
Resident Physician Grant programs. Research by the Association of American
Medical Colleges shows that physicians tend to stay and practice medicine in the
area where they trained.
93
The 2016 National Health Service Corps Participant
Satisfaction Survey found that 88 percent of participating clinicians who received
loan repayment assistance in exchange for working in underserved areas stayed in
that area for up to one year after their obligation, and 43 percent intended to stay
for five or more years.
94
Expanding the loan repayment programs to include more
health professions could increase the number of people practicing other health
professions in underserved areas and incentivize people to enter a health
profession. These programs should also be advertised to expand their reach.
Support new and innovative ways to bring health care providers to rural
areas.
Rural Americans live an average of 10.5 miles from the nearest hospital, compared
to 4.4 miles for those in urban areas.
95
By supporting alternative methods of
bringing health care providers into rural areas, more patients in underserved areas
could receive care. Programs like Care Van, a collaboration between the Caring
Foundation of Texas and other institutions including the Texas Tech University
Health Sciences Center, brings health care providers to communities, including rural
communities, at no cost to those who qualify.
96
The availability of teleservices must also expand to ensure greater access to health
care services. There are currently numerous barriers to the practice of telehealth
and telemedicine. House Bill 5, 87
th
Legislature, Regular Session, 2021, established
a Broadband Development office to improve access to broadband services in rural
areas.
97
A Texas A&M University report identified telemedicine as a way for rural
residents to access subspecialist services and for expanding services offered by
nurse practitioners and physician assistants.
62
Ensure that high school students are educated about the health care
system and careers in health care.
Health care workers from rural areas are more likely to practice in rural areas.
Therefore, high school students in rural areas should be encouraged to enter the
30
health care field.
98
They can be provided with education about how the health care
system works, what careers are available to them in health care, what kind of
preparation is necessary for these careers, and how to apply to training and
educational programs. The Health Professions Recruitment and Exposure at the
University of Texas Southwestern Medical Center accomplishes these goals by
“expos[ing] high school students to medicine and science through a variety of
workshops and hands-on activities.”
99
High schoolers can also begin their path toward professional licensure. Seven
vocational nursing programs in Texas offer options for high school students to take
nursing courses and become licensed shortly after high school graduation.
100
Supporting programs for high school students could increase prospective entrants
into health care fields experiencing workforce shortages.
31
5. Mental Health and Behavioral Health
Workforce
This section covers the growing need for U.S. and Texas mental health services for
distinct demographic categories. In addition, it discusses and displays the shortages
of the behavioral health workforce and the challenges faced for recruitment and
retention.
Background
Nationally, almost half of adults (46.4 percent) will experience a diagnosable
mental disorder in their lifetime.
101
On an annual basis, over one in four adults
(26.2 percent) in the U.S. experience mental illness and about one in 17 (5.8
percent) experience a serious mental illness.
102
Half of diagnosable mental disorders
begin by the age of 14 and three-fourths begin by the age of 24.
101
Moreover, an
estimated 14 to 20 percent of young people annually have mental, emotional, and
behavioral disorders.
103
According to the 2020 National Survey on Drug Use and Health, 52.9 million adults
aged 18+ (21.0 percent) experienced mental illness and 14.2 million adults (5.6
percent) experienced serious mental illness in the past year.
104
Among children and
adolescents aged 12 to 17, 4.1 million (17.0 percent) experienced a major
depressive episode and 2.9 million (12.0 percent) experienced a major depressive
episode with severe impairment in the past year.
The 2020 survey results also indicate that only 46.2 percent of adults who
experienced mental illness and 64.5 percent of adults who experienced serious
mental illness in the U.S. received inpatient or outpatient mental health services or
took prescription medication for a mental health condition in the past year.
Furthermore, an unmet need for mental health services in the past year was
perceived by 30.5 percent of adults who experienced mental illness and 49.7
percent of adults who experienced serious mental illness. Among children and
adolescents aged 12 to 17 who experienced a major depressive episode, just 41.6
percent received treatment for depression in the past year.
Additionally, the 2020 survey results indicate that the COVID-19 pandemic
negatively affected mental health. From October to December 2020, the majority of
adults (73.0 percent) and the majority of children and adolescents aged 12 to 17
32
(69.1 percent) in the U.S. perceived that the COVID-19 pandemic had a negative
effect on their mental health. For adults as well as children and adolescents aged
12 to 17, 18.3 percent perceived that their mental health was negatively affected
“quite a bit or a lot” because of the COVID-19 pandemic. Another 54.7 percent of
adults and 50.8 percent of children and adolescents perceived that their mental
health was negatively affected “a little or some” because of the COVID-19
pandemic.
A national study conducted by the Center for Studying Health System Change found
that 66.8 percent of primary care physicians were unable to refer their patients to
high-quality outpatient mental health services.
105
This percentage of unavailability
is much higher than the percentages reported by primary care physicians for other
common referrals, including high-quality specialist referrals (33.8 percent), high-
quality imaging services (29.8 percent), and nonemergency hospital admissions
(16.8 percent). Primary care physicians reported that the unavailability of high-
quality outpatient mental health services was due to lack of or inadequate health
insurance coverage, a shortage of providers, and health plan barriers.
Despite the established need for mental health services, a mental health workforce
shortage is evident nationwide. According to the Health Resources and Services
Administration (HRSA), over 148.2 million people in the U.S. live in the 6,222
HPSA’s for mental health.
106
Areas designated by HRSA as HPSA’s for mental health
may be based on the ratio of population to psychiatrist, the ratio of population to
core mental health provider (includes psychiatrists, clinical psychologists, clinical
social workers, psychiatric nurse specialists, and marriage and family therapists), or
both of these ratios.
● If based on the ratio of population to psychiatrist, geographic designations
must have a ratio of 30,000 to 1. In areas with high needs,
e
geographic
designations or population designations must have a ratio of 20,000 to 1.
● If based on the ratio of population to core mental health provider, geographic
designations must have a ratio of 9,000 to 1. In areas with high needs,
geographic designations or population designations must have a ratio of
6,000 to 1.
e
High needs areas are those that meet specific qualifications on population to provider
ratios, percent of population below the FPL, and/or distance to health care. More
information can be found at
Scoring Shortage Designations | Bureau of Health Workforce
(hrsa.gov).
33
● If based on the ratios of both population to psychiatrist and population to
core mental health provider, geographic designations must have a population
to psychiatrist ratio of 20,000 to 1 and a population to core mental health
provider ratio of 6,000 to 1. In areas with high needs, geographic
designations or population designations must have a population to
psychiatrist ratio of 15,000 to 1 and a population to core mental health
provider ratio of 4,500 to 1.
Most HPSA’s for mental health are designated based on the ratio of population to
psychiatrist. Estimates show that an additional 7,420 mental health providers would
be needed to remove the existing health professional shortage area designations
for mental health in the U.S.
Demand for mental health services is projected to increase nationwide due to the
aging population.
107
The number of older adults with mental and behavioral health
problems is projected to increase by 11 million from 1970 to 2030. Moreover, the
aging of the national population requires behavioral health service providers with
special knowledge and skills.
108
HRSA issued national-level supply and demand projections for several behavioral
health occupations from 2016 to 2030 that incorporate estimates of unmet need for
behavioral health services. These projections are based on the unlikely assumption
that there are no changes in the levels of behavioral health care service provision or
utilization from 2017 to 2030. Based on these projections, there will be an
estimated shortage of 34,940 addiction counselors,
109
21,150 adult psychiatrists,
14,300 clinical, counseling, and school psychologists, and 40,140 mental health
counselors nationwide in 2030. These projections also indicate that there will be an
estimated surplus of 3,720 child and adolescent psychiatrists, 1,650 marriage and
family therapists, 2,440 psychiatric nurse practitioners, 1,500 school counselors,
and 200,280 social workers nationwide in 2030.
Workforce-based explanations for an inadequate supply of mental health and
addiction providers at-large generally focus on insufficient numbers of providers,
high turnover, low compensation, a lack of diversity, and limited competency in
evidence-based treatments.
108
Describing the mental health workforce shortage
quantitatively can be problematic, as relevant data have not been universally
collected and there is no agreed-upon definition of adequate supply.
110
However,
efforts to describe the mental health workforce shortage should consider both the
population’s need for mental health services and the number of providers available
to deliver these services.
34
Texas’ Need for Mental Health Services
As noted above, one part of describing a workforce shortage involves
demonstrating the needs of the population for mental health services. A standard
definition of mental health need is not available at the state or national level.
Children
No reliable statewide survey data on mental health needs exist for children younger
than high school age. However, data from HHSC indicate that 44,031 children who
were 13 years of age or younger received mental health services from local mental
health authorities in Texas during state fiscal year 2017.
111
The top five diagnostic
groups were attention deficit disorder (53 percent), adjustments/other non-
psychotic (9 percent), disruptive behavior disorder (8 percent), affective disorders -
other (8 percent), and affective disorders - major depression (6 percent).
Adolescents
According to the 2019 Texas Youth Risk Behavior Survey, 38.3 percent of Texas
high school students reported feeling so sad or hopeless almost every day for at
least two weeks in the past year that they stopped doing some usual activities.
112
Similar results were reported by age and grade level where high school students 18
years of age and older (46.1 percent) were significantly more likely to report feeling
so sad or hopeless almost every day for at least two weeks in the past year that
they stopped doing some usual activities than those 15 years of age and younger
(34.7 percent). Twelfth graders (43.2 percent) were significantly more likely to
report such than ninth graders (32.7 percent). Females (48.6 percent) were
significantly more likely to report these feelings than males (28.3 percent). No
significant differences were reported by race/ethnicity.
The 2019 survey results also indicate that 18.9 percent of Texas high school
students reported seriously considering a suicide attempt in the past year. Females
(25.3 percent) were significantly more likely to report seriously considering a
suicide attempt in the past year than males (12.6 percent), and those in the
“Other” races/ethnicities category (25.5 percent) were significantly more likely to
report such than Hispanics (16.7 percent). No significant differences were reported
by age or grade level. In addition, 15.0 percent of Texas high school students
reported making a plan in the past year for how they would attempt suicide. While
there were no major differences reported by age, grade level, or race/ethnicity,
females (19.4 percent) were significantly more likely to report making a plan in the
past year for how they would attempt suicide than males (10.6 percent). Results
35
further indicate that 10.0 percent of Texas high school students reported
attempting suicide at least once in the past year and 3.4 percent reported requiring
medical treatment after doing so. No major differences were reported by age,
gender, grade level, or race/ethnicity.
The percentage of Texas high school students who reported feeling sad or hopeless,
seriously considering a suicide attempt, making a suicide plan, attempting suicide,
and requiring medical treatment following a suicide attempt increased significantly
from 2009 to 2019. No significant differences were found between Texas high
school students and high school students nationwide in the likelihood of reporting
feeling sad or hopeless, seriously considering a suicide attempt, making a suicide
plan, attempting suicide, or requiring medical treatment following a suicide attempt
in 2019.
Adults
The 2020 results from the Texas Behavioral Risk Factor Surveillance System
15
indicate increases in all categories displayed here as compared to the 2018
results.
111
Just over 23 percent of Texas adults reported having poor mental health
for five or more days in the past 30 days. Adults between 18 and 29 years (33.8
percent) were significantly more likely to report having poor mental health for five
or more days than those between the ages of 45 and 64 (21.1 percent) and adults
who are 65+ years (13.7 percent). Moreover, adults between 30 and 44 years
(21.3 percent) and adults between 45 and 64 years were significantly more likely to
report having poor mental health for five or more days than those 65+ years (10.3
percent). Results by gender indicate that females (27.9 percent) were significantly
more likely to report having poor mental health for five or more days than males
(18.4 percent). No significant differences were reported by race/ethnicity.
Additionally, 13.2 percent of Texas adults reported having poor mental health for
14 or more days in the past 30 days. No significant differences were reported by
age, gender, or race/ethnicity.
The 2020 survey results also indicate that 17.7 percent of Texas adults reported
ever being told by a doctor, nurse, or other health professional that they had a
depressive disorder, including depression, major depression, dysthymia, or minor
depression.
Females (22.5 percent) were significantly more likely to report ever
being told by a doctor, nurse, or other health professional that they had a
depressive disorder than males (12.7 percent), and whites (21.2 percent) were
significantly more likely to report such than Hispanics (14.8 percent). No significant
differences were reported by age.
36
Texas’ Mental Health Workforce
In addition to patient need, a shortage of providers determines the insufficiency of
the mental health workforce. The supply of providers can be conceptualized as
being composed of two broad determinants. The first is the entire number of
providers qualified to serve in mental health, and the second is the number of those
providers committed to providing patient care and the percentage of their
productive time committed to doing so.
113
DSHS uses the population to psychiatrist ratio that is at least 30,000 to 1 or, in
areas with high needs, 20,000 to 1 to apply for HPSA’s for mental health through
HRSA. As of June 2020, 236 of the 254 counties (92.9 percent) in Texas were
wholly or partially designated as a HPSA for mental health.
114
Moreover, as of
September 2019, 173 counties (68.1 percent) in Texas had no psychiatrists.
The state’s mental health workforce shortage is expected to worsen, as the
workforce is aging and many providers are nearing retirement age. At the same
time, educational institutions in the state and the nation are not producing enough
new graduates to meet projected demand. Given the nationwide mental health
workforce shortage, it is unlikely that Texas can meet its staffing needs by
recruiting providers from other states.
115
DSHS issued a report in 2020 projecting the supply and demand for all physicians
and 35 physician specialties in Texas from 2018 through 2032.
116
Statewide results
from this report indicate that there will be an estimated shortage of 1,043 full-time
equivalent psychiatrists by 2032.
In addition to a shortage of providers, other sociodemographic factors contribute to
the state’s inadequate mental health workforce. For example, mental health
providers are not distributed evenly across the state, resulting in differential access
to care by region, especially in rural areas and along the border. Further, the
mental health provider workforce does not reflect the state’s growing racial/ethnic
diversity, resulting in the continued need for culturally competent mental health
care.
Mental Health Workforce by Profession Among
Racial/Ethnic Categories, Texas, 2019
The racial/ethnic distribution of Texas’ mental health workforce differed greatly
from that of the Texas population in 2021. The composition of Texas’ population
37
was estimated to be 40.5 percent white, 40.0 percent Hispanic/Latino, 12.0 percent
African American, and 7.5 percent from other races/ethnicities. Yet, whites were
overrepresented in the majority of mental health professions when compared to the
Texas population. However, over 60 percent of community health workers or
promotores were Hispanic or Latino and 22 percent were African American, which
were larger proportions than within any other profession. Whites were
overrepresented in psychiatry by 13 percentage points and people in the “Other”
category by 22 percentage points.
Overview of Mental Health Workforce by Profession
The tables below are based on licensure data that
117
DSHS receives annually from
the respective state licensing board for the following professions: clinical nurse
specialists, community health workers or promotores, licensed baccalaureate social
workers, licensed chemical dependency counselors, licensed clinical social workers,
licensed master social workers, licensed professional counselors, licensed
psychological associates, licensed psychologists, licensed specialists in school
psychology, marriage and family therapists, nurse practitioners, provisionally
licensed psychologists, and psychiatrists.
Counts include only providers who were licensed with their Texas board and actively
working in their profession. Clinical nurse specialists and nurse practitioners include
only those who indicated they were employed in the field of nursing and had a
specialty in psychiatric/mental health. Psychiatrists include only those who
indicated they provided direct patient care. Analyses include all providers for whom
the respective data were available.
38
Table 2. Number of Providers and Population to Provider Ratio of Mental Health
Workforce by Profession, Texas, 2021
Profession
Number of
Providers
Population to
Provider Ratio
Clinical Nurse Specialists
f
152 192,061.0
Community Health Workers or
Promotores
4,515 6,681.9
Licensed Baccalaureate Social Workers 3,623 8,327.1
Licensed Chemical Dependency
Counselors
5,999 5,029.0
Licensed Clinical Social Workers 9,262 3,257.3
Licensed Master Social Workers 11,310 2,667.5
Licensed Professional Counselors 23,043 1,309.2
Licensed Psychological Associates 813 37,108.2
Licensed Psychologists 4,955 6,088.6
Licensed Specialists in School Psychology 3,748 8,049.3
Marriage and Family Therapists 2,955 10,209.5
Nurse Practitioners
f
1,002 29,135.0
Psychiatrists 2,438 12,374.5
Using 2021 population projections from the Texas Demographic Center and the
total number of providers in Texas, licensed professional counselors had the lowest
f
Nursing professions data for nurse practitioners and clinical nurse specialists were only
available for years 2016-2019. Figures for these professions are from 2014.
39
population to provider ratio statewide in 2021, followed by licensed master social
workers and licensed clinical social workers.
Table 3. Percentage of Providers and Population to Provider Ratio of Mental Health
Workforce by Profession for Most and Least Populous Counties, Texas, 2021
Profession
Percentage
of Providers -
Five Most
Populous
Counties
Population to
Provider
Ratio - Five
Most
Populous
Counties
Percentage
of Providers -
249 Least
Populous
Counties
Population to
Provider
Ratio - 249
Least
Populous
Counties
Clinical Nurse
Specialists
f
61.8% 138,427 38.2% 278,984.9
Community
Health Workers
or Promotores
50.4% 5,916.8 49.6% 6,019.9
Licensed
Baccalaureate
Social Workers
29.6% 12,567.6 70.4% 6,545.1
Licensed
Chemical
Dependency
Counselors
43.6% 5,146.1 56.4% 4,938.3
Licensed Clinical
Social Workers
58.6% 2,482.9 41.4% 4,352.6
Licensed Master
Social Workers
54.7% 2,177.5 45.3% 3,259.1
Licensed
Professional
Counselors
45.6% 1,283.5 54.4% 1,330.8
40
Profession
Percentage
of Providers -
Five Most
Populous
Counties
Population to
Provider
Ratio - Five
Most
Populous
Counties
Percentage
of Providers -
249 Least
Populous
Counties
Population to
Provider
Ratio - 249
Least
Populous
Counties
Licensed
Psychological
Associates
50.6% 32,779.8 49.4% 41,533.4
Licensed
Psychologists
63.2% 4,300.2 36.8% 9,163.8
Licensed
Specialists in
School
Psychology
48.6% 7,390.3 51.4% 8,673.5
Marriage and
Family Therapists
54.3% 8,394.1 45.7% 12,794.2
Nurse
Practitioners
f
56% 23,194.5 44% 36,691.9
Psychiatrists 61.7% 8,963.7 38.3% 17,857.2
Texas’ mental health workforce is not evenly distributed throughout the state. In
2021, the state’s five most populous counties (Harris, Dallas, Tarrant, Bexar, and
Travis) had roughly 44.6 percent of the population. The majority (9 out of 13) of
mental health professions had over half of their workforce in these five counties.
41
Table 4. Growth Trends of Mental Health Workforce by Profession, Texas, 2016-
2021
Profession
Average Annual
Growth Rate -
Number of
Providers
Average Annual
Growth Rate -
Population to
Provider Ratio
Clinical Nurse Specialists
f
(5%)
g
(7.1%)
Community Health Workers or
Promotores
3.2% (1.4%)
Licensed Baccalaureate Social Workers (6.3%) 8.9%
Licensed Chemical Dependency
h
Counselors
Not available Not available
Licensed Clinical Social Workers 4.7% (2.9%)
Licensed Master Social Workers 2.8% (1.0%)
Licensed Professional Counselors 4.9% (3%)
Licensed Psychological Associates (1.9%) 3.7%
Licensed Psychologists 2.4% (0.7%)
g
Parentheses in this table indicate a decrease.
h
Data to calculate annual growth rates of licensed chemical dependency counselors
between 2016 and 2021 were unavailable. However, available data show that the number of
active licensed chemical dependency counselors in Texas has increased 17.8 percent since
2014. Available data also show that, relative to population growth, the size of the licensed
chemical dependency counselor workforce has improved by 8.8 percent over the past five
years.
42
Profession
Average Annual
Growth Rate -
Number of
Providers
Average Annual
Growth Rate -
Population to
Provider Ratio
Licensed Specialists in School Psychology 3.1% (1.4%)
Marriage and Family Therapists 1.7% (0.05%)
Nurse Practitioners
f
21.6% 16.0%
Psychiatrists 2.9% (1.2%)
Among the 13 mental health professions for whom annual growth rates between
2016 and 2021 were available, nine professions had an increase in the average
annual growth rate for the number of providers in Texas. When considering
population growth, only three of these 13 mental health professions had an
improvement in the size of the workforce over these five years.
43
Table 5. Number of Counties with No Providers of Mental Health Workforce by
Profession, Texas, 2016-2021
Profession 2016 2021
Clinical Nurse Specialists
f
208 218
Community Health Workers or
Promotores
131 112
Licensed Baccalaureate Social Workers 52 63
Licensed Chemical Dependency
Counselors
82 78
Licensed Clinical Social Workers 114 91
Licensed Master Social Workers 79 74
Licensed Professional Counselors 46 37
Licensed Psychological Associates 153 168
Licensed Psychologists 143 147
Licensed Specialists in School Psychology 166 105
Marriage and Family Therapists 132 112
Nurse Practitioners
f
206 185
Psychiatrists 173 168
Many counties in Texas do not have any providers for at least one mental health
profession. The number of counties in the state with no providers increased for four
mental health professions between 2016 and 2021, while the number of counties in
the state with no providers decreased for nine mental health professions.
44
Table 6. Percentage of Mental Health Workforce by Profession Eligible for
Retirement in 10 Years, Texas, 2021
Profession 56-65 Years Over 65 Years Total
i
Clinical Nurse Specialists
f
32.9% 59.9% 92.8%
Community Health Workers
or Promotores
10.8% 4.9% 15.7%
Licensed Baccalaureate
Social Workers
25.9% 11.6% 37.5%
Licensed Chemical
Dependency Counselors
27.3% 18.9% 46.2%
Licensed Clinical Social
Workers
16.9% 16.4% 33.3%
Licensed Master Social
Workers
10.3% 5.9% 16.2%
Licensed Professional
Counselors
17.2% 16.4% 33.6%
Licensed Psychological
Associates
24.1% 24.4% 48.5%
Licensed Psychologists 17.2% 25.6% 42.8%
Licensed Specialists in
School Psychology
10.9% 11.6% 22.5%
Marriage and Family
Therapists
18.6% 29.5% 48.1%
Nurse Practitioners
f
14.5% 5.7% 20.2%
Psychiatrists 21.6% 24.4% 46%
i
Calculations in the total column are based on unrounded numbers.
45
Policy Recommendations for the Legislature,
the Governor, and Executive Branch Agencies
Support efforts by school districts to increase access to mental health
services for students.
Increasing the number of counselors and psychologists employed by school districts
in the state is one way that school districts may increase access to mental health
services for students. Generally, the recommended student to provider ratio differs
based on the profession. For example:
● The American School Counselor Association recommends a student to school
counselor ratio of 250 to 1.
118
● The National Association of School Psychologists recommends a student to
school psychologist ratio between 500 to 1 and 700 to 1.
119
According to the Texas Education Agency, there were 13,864 full-time equivalent
counselors and 2,089 full-time equivalent licensed specialists in school psychology
or psychologists employed by school districts in Texas during the 2020-2021 school
year.
120
Based on the statewide enrollment of 5,371,586 students, there was a
student to counselor ratio of 387.4 to 1 and a student to licensed specialist in
school psychology or psychologist ratio of 2,570.4 to 1 for the 2020-2021 school
year.
121
As the statewide ratios for counselors and licensed specialists in school psychology
or psychologists employed by school districts exceed the ratio recommended by the
respective professional association listed above, it is important that school districts
consider increasing the number of counselors and psychologists that they employ.
Moreover, additional providers employed by school districts would better ensure
that students have access to mental health services in the school setting.
Another way that school districts in the state may increase access to mental health
services for students is to partner with community mental health centers. Currently,
school districts are not required to provide mental health services to students or to
partner with community mental health centers in providing such services. As not all
school districts have prioritized providing mental health services, many students
throughout the state may not have access to mental health services in the school
setting.
46
Due to the challenge of providing mental health services and the limited resources
of many school districts, particularly in rural areas, it is important that school
districts not be burdened with creating their own infrastructure for providing mental
health services. In addition, solutions should be developed that leverage existing
services. As community mental health centers already have the staff, training, and
experience necessary to help students, partnering with them would allow school
districts to take advantage of existing services in a cost-effective manner.
Furthermore, it may not be necessary for every school district to have a full-time
mental health provider. Partnering with community mental health centers would
allow school districts, especially those that do not provide mental health services, to
increase access to cost-effective mental health services for students.
Post-secondary students face their own challenges on campus. A 2021 study
reported that suicide is the third leading cause of death in students and that up to
44 percent of college students reported having symptoms of depression and
anxiety.
122
Additionally, of those who have been diagnosed with a mental health
disorder, most (75 percent) have their first episode by age 24. Texas A&M
University conducted a study in 2020 of the effects of COVID-19 on college
students’ mental health.
123
They found that 71 percent of undergraduate students
reported experiencing increased stress and anxiety due to the COVID-19 pandemic.
Of those students, 91 percent were concerned about the health of their loved ones
and themselves, 89 percent experienced difficulty concentrating, 86 percent
reported disruptions to sleeping patterns, 86 percent reported decreased social
interactions due to physical distancing, and 82 percent reported increased concerns
on academic performance. Nationally and statewide, college and university students
are facing complex mental health issues.
Continue outreach efforts to de-stigmatize behavioral health, and for
resources for mental health providers for students.
According to the 2019 Texas Youth Risk Behavioral Survey results, 10 percent of
Texas high school students attempted suicide, and 38.3 percent felt sad or hopeless
for two weeks in a row within the year leading up to the survey.
124
The lack of
outreach, resources, and efforts to normalize mental health in schools has led to
the isolation of students struggling with mental health issues. In addition to the
recommendation above, schools should create curriculum on mental health topics
and incorporate this knowledge into classes, campaigns, and assemblies that invite
47
experts on relevant mental health topics. The de-stigmatization of mental health
challenges will decrease the barriers to improving mental health for students.
Continue to support the work of the Texas Child Mental Health Care
Consortium (TCMHCC).
Senate Bill 11, 86th Legislature, Regular Session, 2019, established the TCMHCC.
125
Members of the consortium include 13 health-related institutions of higher
education, HHSC, the Texas Higher Education Coordinating Board, and three
nonprofit organizations that focus on mental health care.
126
These nonprofit
organizations currently include the Meadows Mental Health Policy Institute, the
Hogg Foundation for Mental Health, and the Texas Council of Community Health
Centers.
127
The consortium is governed by an executive committee.
128
The purpose of the consortium is to:
● Leverage the expertise and capacity of the 13 health-related institutions of
higher education to address urgent mental health challenges and improve the
mental health care system in the state in relation to children and
adolescents; and
● Enhance the state's ability to address the mental health care needs of
children and adolescents through collaboration of the 13 health-related
institutions of higher education.
129
The consortium is tasked with the following initiatives:
● Establish a network of comprehensive child psychiatry access centers; and
● Establish or expand telemedicine or telehealth programs to identify and
assess behavioral health needs and provide access to mental health care
services.
In addition, the executive committee is authorized to provide funding to any of the
13 health-related institutions of higher education for the purpose of expanding the
state’s child mental health workforce.
130
Such funding may be provided to expand
the child psychiatry workforce and/or to add a child and adolescent psychiatry
fellowship.
The 2022-23 General Appropriations Act, Senate Bill 1, 87
th
Legislature, Regular
Session, 2021, increased the TCMHCC funding, which allocated $19.5 million in
funds for the TCMHCC to support the Child Psychiatry Access Network and the
Texas Child Health Access Through Telemedicine initiatives.
131
48
As the initiatives of the TCMHCC have the ability to improve access to mental health
services for children and adolescents throughout the state, it is imperative that the
work of the consortium continue to be supported. Such support will better ensure
that the state is able to address the mental health care needs of children and
adolescents.
Continue to support the work of the Statewide Behavioral Health
Coordinating Council.
The 2016-17 General Appropriations Act, House Bill 1, 84th Legislature, Regular
Session, 2015 (Article IX, Section 10.04), established the Statewide Behavioral
Health Coordinating Council.
132
Members of the council include representatives of
state agencies and institutions of higher education that receive state funding to
provide behavioral health services. The purpose of the council is to ensure a
strategic statewide approach to behavioral health services.
133
The council is
primarily charged with the following duties:
● Develop and monitor the implementation of a five-year statewide behavioral
health strategic plan;
● Develop a biennial coordinated statewide behavioral health expenditure
proposal; and
● Annually publish an updated inventory of behavioral health programs and
services that are funded by the state that includes a description of how those
programs and services further the purpose of the statewide behavioral health
strategic plan.
House Bill 4074, 87
th
Legislature, Regular Session, 2021, called for the assembling
of a subcommittee on suicide prevention and the inclusion of a suicide prevention
plan in the Statewide Behavioral Health Strategic Plan.
134
In the Texas Statewide Behavioral Health Strategic Plan, Fiscal Years 2017-2021,
the behavioral health workforce shortage was identified as one of the gaps in the
state’s behavioral health system.
135
As the Statewide Behavioral Health
Coordinating Council is addressing the state’s mental health workforce shortage, it
is imperative that the work of the council continue to be supported. Such support
will allow the council to further develop strategies that may improve access to the
state’s behavioral health system.
Support efforts to increase the funding and stipends available to students
of the mental health professions as they complete their education and
training.
49
Completing the education and training required to become a mental health provider
is a timely and expensive process. To lessen the financial burden faced by students
of the mental health professions, consideration should be given to expanding the
funding and stipends available to them as they complete their education and
training. By expanding such funding and stipends, more individuals may be
incentivized to select a mental health profession, likely leading to an increase in the
state’s mental health workforce.
Support the expansion of the Loan Repayment Program for Mental Health
Professionals.
To recruit individuals to the state’s mental health workforce and to retain the
existing mental health workforce, it is important to expand practice incentives for
mental health providers. One practice incentive that could be expanded is the Loan
Repayment Program for Mental Health Professionals that is administered by the
Texas Higher Education Coordinating Board.
136
The eligibility criteria for this
program could be expanded to include additional practice specialties, practice
areas, and/or types of recipients that receive care. For example:
● The practice specialties of mental health providers could be expanded to
include licensed psychological associates, licensed specialists in school
psychology, provisionally licensed psychologists, licensed baccalaureate
social workers, licensed master social workers, and/or community health
workers or promotores.
137
● The practice location of mental health providers could be expanded to include
areas not designated by HRSA as HPSA’s for mental health.
138
● The types of recipients that receive care from mental health providers could
be expanded to include individuals who receive mental health services but
are not:
Enrolled in Medicaid;
Enrolled in CHIP;
Committed to a secure correctional facility operated by or under contract
with the Texas Juvenile Justice Department; and/or
Confined in a secure correctional facility operated by or under contract
with any division of the Texas Department of Criminal Justice.
The funding for the Loan Repayment Program for Mental Health Professionals could
also be expanded. Doing so could improve the efficacy of the program, as new
program participants may be able to enroll in the program sooner and the overall
number of mental health providers participating in the program may increase.
50
By expanding the eligibility criteria and/or funding for the Loan Repayment Program
for Mental Health Professionals, the ability to recruit and retain mental health
providers would be strengthened. Moreover, given that the state’s mental health
workforce is aging and many providers are nearing retirement age, it is imperative
that measures are taken to encourage and incentivize individuals to enter a mental
health profession.
Support expanding the reciprocity of licenses for behavioral health
providers between states.
The process of obtaining a license in a new state can be difficult for licensed mental
health providers who are transitioning from one state to another. This process can
require a considerable amount of time to complete and be cumbersome to navigate
due to states having different requirements. To ease the process for licensed
mental health providers seeking to relocate to Texas and become licensed by the
state, it is important to expand the reciprocity standards between states. Doing so
may lead to an increase in the state’s mental health workforce and, thus, greater
access to mental health services in the state.
Support the increase of reimbursement rates for behavioral health
providers.
The current payment system is a key barrier that affects the recruitment and
retention of mental health providers in the state. As the current payment system
fails to adequately reimburse mental health providers, many providers are not able
to sustain providing mental health services and/or expand their capacity of doing
so. To lessen this barrier, consideration should be given to increasing
reimbursement rates for mental health providers. By increasing such rates, the
state would strengthen its ability to recruit and retain mental health providers, as
well as better ensure access to mental health services throughout the state.
Increase the amount of education on suicide prevention for students
within health care fields.
Often times, health care providers and first responders are the personnel that
patients first see before they see a psychiatrist, psychologist, social worker,
counselor, or other behavioral health provider. Providing more education on suicide
prevention, depression, and anxiety for primary care providers, nurses, and first
responders would allow for more detection of these conditions and for patients to
receive the care needed. Additional options could include questions between patient
and provider at annual physicals or routine appointments and additional intake
51
forms prior to an appointment to detect issues before they increase in severity for
the patient. HRSA has allocated federal funding toward colleges and universities
that educate the medical health care workforce to more holistically educate them
on the diverse needs of each patient.
139
The continuation and expansion of these
types of resources would allow the Texas health care workforce to detect and treat
mental health issues before they become exacerbated.
Monitor the effects of the COVID-19 pandemic on behavioral health in
Texas.
Texans’ mental and behavioral health faced tremendous challenges around access
to care before the COVID-19 pandemic. Overall, Texans had a greater percentage
of people who faced symptoms of anxiety disorder or depressive disorder (34.5
percent) than nationally (31.5 percent).
140
Younger age groups had more symptoms
of anxiety and depression, 48.4 percent of the 18-29 age category reporting
anxiety and depression symptoms, while 17.8 percent of people over 80 reporting
symptoms. Nationally, 14.5 percent (40.3 million) of people aged 12 and over faced
substance abuse disorder in 2020.
104
HHSC estimates that 11.3 million Texans are
living with substance use disorder.
141
There is a general gap in data surrounding
Texans facing substance use disorder during the COVID-19 pandemic. During 2020,
Texas fell below national rates of drug overdose deaths per 100,000 people at 14.3
versus 28.3, respectively.
142
Expanding the processes, methods, and technology for
data collection would improve our insights into Texans’ mental and behavioral
health trends. It is imperative that this work obtains support, as statistics often
contribute to how compelling research is communicated to institutions and
legislative entities, and more mental and behavioral health services would be able
to reach Texans.
Having access to data during different stages of the COVID-19 pandemic has
granted Texas mental and behavioral health care institutions the ability to adapt to
needs within their communities. During the onset of the COVID-19 pandemic, HHSC
launched a mental health support line in an effort to help Texans gain access to
mental health services.
143
The COVID-19 Mental Health Support Line (833-986-
1919) has provided information on the ongoing COVID-19 pandemic, direct access
to local mental and behavioral health authorities, statewide testing and vaccine
information, and referrals to resources through 2-1-1 (essential services provided
through United Way). In 2022, HHSC launched a $23.3 million substance use
prevention awareness campaign with the goal of reducing drug use among Texas
youth and families. Without data on the continuing effects of the COVID-19
pandemic on the mental and behavioral health of Texans, services like these would
52
not exist. The data, accuracy, methods, procedures, and reports could better serve
health care institutions and Texans with investment for further examination.
Continue to support the investment in recruitment and retention of the
mental and behavioral health care workforce.
The mental and behavioral health care workforce shortage has persisted in Texas
since before the COVID-19 pandemic. The Statewide Behavioral Health
Coordinating Council’s December 2020 report states that workforce shortage has
been a decades-long issue.
144
The plan details the short, mid, and long-term action
items surrounding the retention and recruitment of behavioral health care
providers. The Statewide Behavioral Health Coordinating Council formed a
subcommittee in 2019 to develop a plan for increasing and improving the workforce
in Texas to better serve people with mental and substance use issues.
Texas faces behavioral workforce shortages in a variety of professions within the
field. When speaking about psychiatrists specifically, demand will continue to
outpace supply by almost two percentage points from the years 2017-2030.
116
HRSA reports that Texas contains 476 mental HPSA’s in the state, meaning those
areas contain a higher ratio than 30,000 to one health professional per region.
145
With the unknown, emerging, and persistent mental and behavioral health issues
Texans are facing, the mental and behavioral health care workforce should be
expanded and supported to the fullest extent.
Allocate funds toward the implementation of the 988 Suicide Prevention
Lifeline.
In February 2021, HHSC received a $180,000 grant from Vibrant Emotional Health
to support the new 988 Suicide Prevention Lifeline.
146
The lifeline will make it easier
for people in crisis to reach someone within their local community for mental health
support and resources. In July 2022, the 988 Suicide Prevention Lifeline replaced
the National Suicide Prevention Lifeline, formerly known as 1-800-273-8255(TALK).
The grant funds will help existent call centers within Texas prepare for
infrastructure needs, additional callers, purchase headsets, phones, and computers,
train and educate staff, and collect data. Increasing the funding of this endeavor
will support launch efforts and continuation.
53
6. Teleservices and Technology
This section discusses the definition, use, and benefits of teleservices in Texas.
Additionally, it includes how teleservices have been expanded due to the COVID-19
pandemic and how teleservices will continue to be used and changed post-
pandemic.
Defining Teleservices
Federal Medicaid defines telemedicine as an alternative to traditional care in which
a patient and provider meet in real time, using both audio and video equipment, at
separate sites.
147
According to the Texas Occupations Code, telemedicine is
required to fulfill the same standard of care that would be applied in an in-person
setting.
148
Telemedicine and telehealth are often used as interchangeable terms. Telemedicine
is defined as “the remote delivery of health care services and clinical information
using telecommunications technology” while telehealth is “used to describe
diagnosis and management, education, and other fields of health care.”
149,150
The
term “teleservices” will be used to include both “telemedicine” and “telehealth” for
the remainder of this section. For information and data relating specifically to
“telemedicine” or “telehealth,” those terms will be applied.
Use of Teleservices in Texas
H.B. 2386, 75
th
Legislature, Regular Session, 1997 allowed medical providers to be
reimbursed for telemedicine services.
151
In 2016, the e-Health Advisory Committee
was established to advise HHSC on “the development, use, and long-range plans
for telemedicine, telehealth, and home telemonitoring services.”
152
The most
common users of these teleservices are those diagnosed with Attention-Deficit
Hyperactivity Disorder (ADHD), followed by schizophrenia, schizoaffective disorder,
and bipolar disorder.
151
Texas Medicaid users were included among those for whom teleservices were
available. While this has been the case for over 20 years, it is only recently that the
service has begun to see wider spread adoption. From 2012 to 2018, there has
been a 119 percent increase in use of teleservices compared to a 338 percent in
overall use of providers offering teleservices. From fiscal year 2018 to 2019, the
54
utilization of telemedicine services increased by 19 percent, telehealth services
increased by 37 percent, and telemonitoring services increased by 23 percent.
151
COVID-19 and the Expansion of Teleservices
On January 31, 2020, a national Public Health Emergency was declared due to the
2019 novel Coronavirus.
153
On March 17, 2020, Governor Greg Abbott announced
an emergency rule to “allow telemedicine visits for patients with state-regulated
plans to be paid the same as in-office visits for insurance purposes.”
154
On
September 25, 2020, this rule was extended through the end of 2020 and
expanded to include other major health insurers in Texas, ensuring that Texans
could continue utilizing telehealth during the pandemic.
155
In 2021, several bills passed and became effective that supported reimbursement
to providers for teleservices. These include, H.B. 4, 87
th
Legislature, Regular
Session, 2021: reimbursement for health programs using telecommunications;
156
S.B. 228, 87
th
Legislature, Regular Session, 2021: relating to the reimbursement of
“claims by certain health benefit plan issuers for telemedicine services and
telehealth services;”
157
and S.B. 434, 87
th
Legislature, Regular Session, 2021:
pertaining to the delivery of “certain health, mental health, and educational services
in this state” through telecommunication or information technology.
158
Other bills
relating to teleservices were also introduced as a result of the pandemic, such as
S.B. 488, 87
th
Legislature, Regular Session, 2021 addressing teledentistry
services.
159
Due to the need and the opportunity to take advantage of teleservices, the number
of teleservices increased drastically after the COVID-19 pandemic began. There was
a 2,840 percent increase in teleservices provided to Texas Medicaid clients in the
first few months of 2020.
160
The data in Figure 1 below includes the number of teleservices provided across all
Medicaid and CHIP programs in Texas. In February of 2020, right before the
COVID-19 virus was detected in Texas, the number of monthly teleservices was
less than 30,000 statewide. A Public Health Disaster Declaration was issued in
Texas in March of 2020 and subsequently the number of monthly teleservices
drastically increased to over 850,000 in April 2020. While teleservices have
decreased from this peak in April 2020, they remain high.
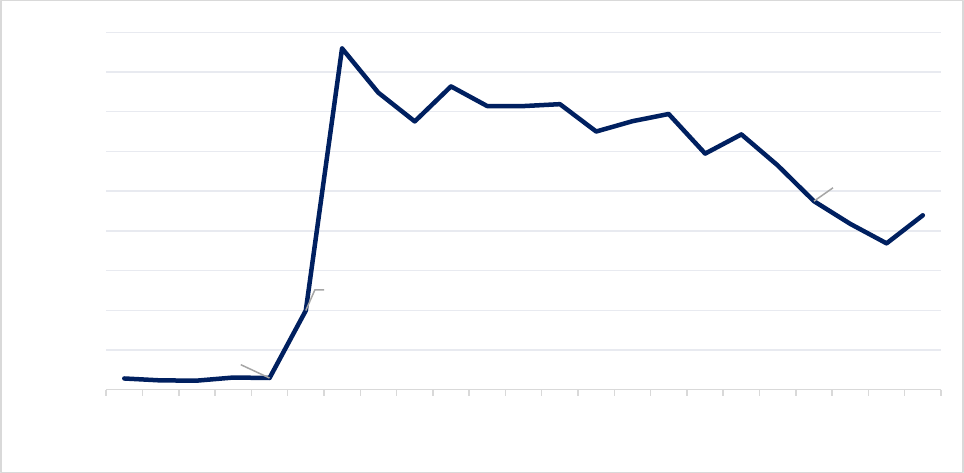
55
Figure 1: Number of Teleservices per Month Under Medicaid and CHIP
161
Benefits of Teleservices
The benefits of teleservices are widespread. For clients of Texas Medicaid who are
blind or have a disability, utilizing teleservices led to less use of inpatient,
outpatient, and emergency department services. Overall, the use of teleservices for
these clients cost $502 less per client per month than using in-person services. It
was also found that overall medical spending for this population increased,
suggesting that teleservices are fulfilling previously unmet needs.
151
Rural areas in Texas also benefit greatly from teleservices. Rural communities often
use teleservices to “augment limited provider resources” caused by losing and
having difficulties recruiting health providers.
160
Teleservices also decrease the
number of no-show patients because factors like childcare, transportation, and
parking are less of an issue.
160
Health providers, through teleservices, are also able
to “assess a patient’s living environment” which can be indicative of certain health
outcomes.
160
A study on medically complex children (children with one or more chronic conditions
that require continuous medical attention) showed that clinical outcomes favored
those using teleservices by 66 to 98 percent, reducing hospital and pediatric
intensive care unit admissions. Teleservices also reduced total health system costs
by 91 percent per child, per year.
162
28,038
29,242
199,325
859,511
675,340
763,843
719,324
650,253
694,077
594,298
643,019
474,736
368,263
438,929
0
100,000
200,000
300,000
400,000
500,000
600,000
700,000
800,000
900,000
Oct-19
Nov-19
Dec-19
Jan-20
Feb-20
Mar-20
Apr-20
May-20
Jun-20
Jul-20
Aug-20
Sep-20
Oct-20
Nov-20
Dec-20
Jan-21
Feb-21
Mar-21
Apr-21
May-21
Jun-21
Jul-21
Aug-21
56
Access to Teleservices
In order to partake in offered teleservices, individuals must have access to
broadband or highspeed internet, access to technologies that can function as audio
and visual tools, and the knowledge to work these technologies.
160,163
Those without
access to these three elements are often the socioeconomically disadvantaged and
those living in rural areas.
Access in Rural Counties
The success of teleservices is dependent on the patient’s access to teleservices and
on the provider’s ability to deliver teleservices. In December 2020, 96 percent of
households in Texas had the option to connect to broadband internet, leaving
316,700 households without that ability.
160
Of those remaining households, 89
percent were considered rural.
160
Without widespread access to broadband, rural
households, specifically those who are socioeconomically disadvantaged, risk being
“left further behind with the increased implementation of telehealth,” due to their
lack of access to necessary technologies.
163
H.B. 5, 87
th
Legislature, Regular
Session, 2021 created “the Broadband Development Office which will award grants
and loans and provide other incentives in the interest of expanding access to
broadband in underserved areas,” enabling rural areas to gain much needed access
to telemedicine.
164
House Bill 76, 87th Legislature, 3rd Special Session was introduced on September
16, 2021, related to a pilot project to provide emergency telemedicine services and
telehealth services in rural areas. The bill ultimately did not pass but the proposed
program would connect emergency providers in rural areas to a call center that
would help determine where the patient needs to go and help the emergency
providers treat them, prehospital, in the field.
165,166
Even with these kinds of
programs being developed in rural areas, the majority of teleservice providers
“continue to be located in large Metropolitan Statistical Areas, such as Dallas-Fort
Worth-Arlington, San Antonio, and Houston-The Woodlands-Sugar Land.”
151
Providers’ Ability to Deliver Teleservices
Another limitation of teleservices is the ability for a provider to offer those services
under existing legislation or regulation. In March of 2020, the Texas Medical
Association released a document outlining the rules and regulations on the
technology, billing, and policies surrounding telemedicine due to the COVID-19
pandemic.
167
57
If a patient travels or moves out of state, they cannot continue seeing their
provider, even through teleservices, if their provider is not licensed in the state of
their physical location. The Interstate Medical Licensure Compact (IMLC) allows
doctors to become licensed in multiple states and is one way a provider can
continue giving care to patients who have moved out of their original state.
168
The
IMLC was launched even before the start of the COVID-19 pandemic, but many
states do not participate.
169
Texas is still in the process of implementing the IMLC
for physicians.
168
Before the pandemic, Health Insurance Portability and Accountability Act (HIPAA)
privacy standards disallowed providers from utilizing more user-friendly platforms
to conduct teleservices. After emergency protocols were put into place during
COVID-19, HIPAA compliance was relaxed and many providers began using
platforms like Skype and FaceTime. As pandemic legislation expires, providers must
use more HIPAA-compliant platforms that are often less accessible to patients,
making it more difficult for these providers to deliver teleservices.
169
Teleservices Post-COVID-19
Two years after the Public Health Emergency was declared, states are beginning to
retighten their rules on teleservices.
169
However, the COVID-19 pandemic forced
many physicians, who had previously never provided teleservices, to begin shifting
their practice to become more teleservice focused. Because of this, “nearly 11,000
additional providers served Medicaid beneficiaries using teleservices, with about
5,000 of this group providing a teleservice to a rural resident.”
160
This increased the
number of physicians experienced in teleservices and increased health care services
in rural areas. Throughout 2022, HHSC will evaluate the feasibility of continuing
certain teleservices that were available under Medicaid and CHIP during the Public
Health Emergency.
170
Legislation was introduced to continue the expansion of teleservices. S.B. 434, 87
th
Legislature, Regular Session, 2021 as discussed in the “Expansion of Telemedicine”
section above requires the executive commissioner to adopt certain rules,
“including rules governing when the delivery of service coordination benefits using
telecommunications or information technology is appropriate.”
158
In Section
403.153 of Senate Bill 434, under “Use of Telecommunication Technology,” license
holders will be able to “provide a service solely through the use of an interactive
audiovisual communication system, whether real-time or two-way, including a
smartphone.” The bill did not pass, but looking towards future sessions, it is
possible that legislation affecting telehealth services will continue to be filed.
58
Ultimately, whether teleservices will continue to be provided and used will depend
on Medicare and private insurance companies continuing to cover them. If Congress
does not extend Medicare’s teleservices coverage, Medicare could begin excluding
teleservices to clients and taking away reimbursement that has helped thousands of
Texans throughout the public health emergency.
160
HHSC’s stakeholders have
“expressed interest in making COVID-19 telemedicine, telehealth, and telephonic
flexibilities permanent benefits of Texas Medicaid.”
151
Policy Recommendations for the Legislature,
the Governor, and Executive Branch Agencies
Continue to expand the Statewide Health Information Exchange and
incentivize its use among third party teleservices agencies.
Many Texans choose third party teleservices agencies when seeking care. Health
Information Exchange programs are utilized by health care providers and enable
better health care coordination, better quality of care, and can also keep health
care costs down.
171
The Health Information Technology for Economic and Clinical
Health Act was enacted in 2009 to incentivize the promotion of health information
technology and exchange.
172
The Texas Health Information Exchange
Implementation Advanced Planning Document defines the funding opportunities for
eligible health professionals who adopt health information exchange systems.
173
These funding mechanisms are supported by Centers for Medicare and Medicaid
Services and may not always reach third party teleservice providers. By connecting
third party teleservice providers with patients’ primary care physicians through
Health Information Exchange programs, the state is ensuring that patients are
receiving quality, safe, and effective care as well as improving public health
reporting and monitoring.
171
Encourage state, federal, and private health insurance organizations to
promote their teleservice benefits.
Teleservices provide an array of benefits for patients, including the elimination of
transportation costs and scheduling flexibility.
167
Benefits also extend to providers
and organizations who can provide more cost-effective care
169
to a larger
population, specifically in rural areas.
166
Many state, federal, and private health
insurance organizations have policies regarding teleservices, including the
reimbursement and steps for utilization. Insurance consumers would benefit from
learning and understanding the services they already have access to.
59
Support new and innovative ways to get teleservices to rural communities.
Getting teleservices to rural communities is essential in ensuring that these
communities have access to health care. With 4 percent, or more than 300,000
households, unable to access broadband internet across Texas,
160
rural
communities need options for teleservices that don’t require this broadband access.
One example is organizations that have provided direct-to-consumer care using
telemedicine kiosks placed in pharmacies in rural areas. These kiosk systems have
been observed to increase health care access without requiring an internet
connection at home.
174
Community Health Workers could also be considered to help
bridge the gap in knowledge needed to access teleservices, especially for the
elderly population.
Investigate the training requirements for teleservice providers to
determine if adequate training is being conducted at health institutions.
As the number of teleservices provided each month remains high, more than ten
times the number of teleservices provided to Medicaid and CHIP recipients in
February 2020,
161
the need for health care providers to be able to deliver these
services is also high. Especially at the beginning of the COVID-19 pandemic,
physicians and other health care providers began providing care through
teleservices, often for the first time. Providers should be trained to deliver
teleservices through their practice to ensure that quality of care is being met.
60
7. List of Acronyms
Acronym Full Name
ACA Affordable Care Act
CHIP Children’s Health Insurance Program
COVID-19 Coronavirus Disease 2019
DSHS Department of State Health Services
DSRIP Delivery System Reform Incentive Payment
EMS Emergency Medical Services
FPL Federal Poverty Level
HHSC Health and Human Services Commission
HIPAA Health Insurance Portability and Accountability Act
HPSA Health Professional Shortage Area
HRSA Health Resource Services Administration
IMLC Interstate Medical Licensure Compact
STAR State of Texas Access Reform
STAR+PLUS State of Texas Access Reform Plus
TCMHCC Texas Child Mental Health Care Consortium

61
Acronym Full Name
TIPPS Texas Incentives for Physician and Professional Service
62
Appendix A. Statewide Health Coordinating Council
Roster
Gubernatorial Appointees Role
Elizabeth Protas, P.T., Ph.D.
Chair, League City
Public Member
Kimberly Haynes, D.M.D, C.A.G.S., F.I.D.I.A.
Leander
Health Care Professional
Emily Hunt, D.N.P
Houston
Hospital Representative
Carol Boswell, Ed.D., R.N., C.N.E., A.N.E.F.,
F.A.A.N.
Andrews
University Representative
Bharath Thankavel, M.D.
Dallas
HMO Representative
Chelsea Elliott
Austin
Public Member
Cheryl Sparks, Ed.D.
Big Spring
Community College Representative
Melinda Rodriguez, P.T., D.P.T.
San Antonio
Health Care Professional
Tamara Rhodes, M.S.
Amarillo
Nurse Representative
D. Bailey Wynne, M.H.A., R.Ph., C.H.E.S.
Dallas
Public Member
Doris Jackson, D.H.A.
Pearland
University Representative
Ken Holland
Huntsville
Public Member
Yasser Zeid, M.D.
Tyler
Health Care Professional
State Agency Members Representing
Jimmy Blanton, M.P.Aff.
Austin
Texas Health and Human Services
Commission
Courtney Harvey, Ph.D.
Austin
Texas Health and Human Services
Commission
63
Aelia Akhtar
Austin
Texas Department of State Health
Services
Elizabeth Mayer, M.P.Aff.
Austin
Texas Higher Education Coordinating
Board
64
8. References
1. Gulliford M, Figueroa-Munoz J, Morgan M, et al. What does “access to health
care” mean? J Health Serv Res Policy. 2002;7(3):186-188.
2. Pandhi N, DeVoe JE, Schumacher JR, et al. Number of First-Contact Access
Components Required to Improve Preventive Service Receipt in Primary Care
Homes. J Gen Intern Med. 2012;27(6):677-684. doi:10.1007/s11606-011-
1955-7
3. Shi L, Lebrun-Harris LA, Daly CA, et al. Reducing Disparities in Access to Primary
Care and Patient Satisfaction with Care: The Role of Health Centers. J Health
Care Poor Underserved. 2013;24(1):56-66.
4. Leveque JF, Harris MF, Russell G. Patient-centred access to health care:
conceptualising access at the interface of health systems and populations. Int J
Equity Health. 2013;12(18). Accessed November 4, 2021.
https://link.springer.com/article/10.1186/1475-9276-12-18
5. Kullgren JT, McLaughlin CG, Mitra N, Armstrong K. Nonfinancial Barriers and
Access to Care for U.S. Adults. Health Serv Res. 2012;47(1):462-485.
doi:10.1111/j.1475-6773.2011.01308.x
6. Neuhausen K, Grumbach K, Bazemore A, Phillips RL. Integrating Community
Health Centers Into Organized Delivery Systems Can Improve Access To
Subspecialty Care. Health Aff (Millwood). 2012;31(8):1708-1716.
doi:10.1377/hlthaff.2011.1261
7. Au M, Taylor EF, Gold M. Improving Access to Language Services in Health Care:
A Look at National and State Efforts. Mathematica Policy Research, Inc.; 2009.
8. Gessert C, Waring S, Bailey-Davis L, Conway P. Rural definition of health: a
systematic literature review. BMC Public Health. 2015;15(378). Accessed
November 4, 2021. https://link.springer.com/article/10.1186/s12889-015-
1658-9
9. Kenney GM, McMorrow S, Zuckerman S, Goin DE. A Decade Of Health Care
Access Declines For Adults Holds Implications For Changes In The Affordable
Care Act. Health Aff (Millwood). 2012;31(5):899-908.
10.Agency for Healthcare Quality Research. 2019 National Healthcare Quality and
Disparities Report. US Department of Health and Human Services; 2020.
Accessed December 29, 2021.
https://www.ahrq.gov/research/findings/nhqrdr/nhqdr19/index.html
11.Flores G, Lin H. Trends in racial/ethnic disparities in medical and oral health,
access to care, and use of services in US children: has anything changed over
the years? Int J Equity Health. 2013;12(10). doi:10.1186/1475-9276-12-10
65
12.Radley DC, Schoen C. Geographic Variation in Access to Care — The Relationship
with Quality. N Engl J Med. 2012;367(1):3-6. doi:10.1056/NEJMp1204516
13.Jan 21 ADP, 2021. The Coverage Gap: Uninsured Poor Adults in States that Do
Not Expand Medicaid. KFF. Published January 21, 2021. Accessed November 4,
2021. https://www.kff.org/medicaid/issue-brief/the-coverage-gap-uninsured-
poor-adults-in-states-that-do-not-expand-medicaid/
14.U.S. Census Bureau. 2016-2020 American Community Survey; Public Use Micro
Data Sample (Texas-Specific).
15.Texas Behavioral Risk Factor Surveillance System 2020.
16.2020 5-Year American Community Survey (Texas-Specific Samples). U.S.
Census Bureau
17.Everyone Included: Social Impact of COVID-19. United Nations Department of
Economic and Social Affairs. Accessed January 20, 2022.
https://www.un.org/development/desa/dspd/everyone-included-covid-19.html
18.Reduced Access to Care During COVID-19 | Data | Centers for Disease Control
and Prevention. Centers for Disease Control and Prevention. Published August 6,
2021. Accessed January 20, 2022. https://data.cdc.gov/NCHS/Reduced-Access-
to-Care-During-COVID-19/th9n-ghnr
19.Dorn S. The COVID-19 Pandemic and Resulting Economic Crash Have Caused
the Greatest Health Insurance Losses in American History. Families USA.
Published July 13, 2020. Accessed January 20, 2022.
https://familiesusa.org/resources/the-covid-19-pandemic-and-resulting-
economic-crash-have-caused-the-greatest-health-insurance-losses-in-american-
history/
20.Garfield R, Claxton G, Damico A, Levitt L. Eligibility for ACA Health Coverage
Following Job Loss - Appendix. Kaiser Family Foundation. Published May 13,
2020. Accessed January 20, 2022. https://www.kff.org/report-section/eligibility-
for-aca-health-coverage-following-job-loss-appendix/
21.Sparber MM and S. As Texas expands COVID-19 vaccination eligibility, racial
disparities persist among Black, Hispanic residents. The Texas Tribune.
https://www.texastribune.org/2021/03/19/texas-vaccine-race-disparities/.
Published March 19, 2021. Accessed January 20, 2022.
22.Ndugga N, Hill L, Artiga S, Sweta H. Latest Data on COVID-19 Vaccinations by
Race/Ethnicity. Kaiser Family Foundation. Published January 12, 2022. Accessed
January 20, 2022. https://www.kff.org/coronavirus-covid-19/issue-brief/latest-
data-on-covid-19-vaccinations-by-race-ethnicity/
23.CDC. COVID Data Tracker. Centers for Disease Control and Prevention.
Published January 1, 2022. Accessed September 29, 2022.
https://covid.cdc.gov/covid-data-tracker
66
24.Texas Health Professions Resource Center Physician 2021 Data.
25.Paradise J, Garfield R. What is Medicaid’s Impact on Access to Care, Health
Outcomes, and Quality of Care? Setting the Record Straight on the Evidence -
Issue Brief. Kaiser Family Foundation. Published August 2, 2013. Accessed
January 21, 2022. https://www.kff.org/report-section/what-is-medicaids-
impact-on-access-to-care-health-outcomes-and-quality-of-care-setting-the-
record-straight-on-the-evidence-issue-brief/
26.Health Insurance Coverage of the Total Population (CPS). Kaiser Family
Foundation. Published September 21, 2021. Accessed January 21, 2022.
https://www.kff.org/other/state-indicator/health-insurance-coverage-of-the-
total-population-cps/
27.Green LV, Savin S, Lu Y. Primary Care Physician Shortages Could Be Eliminated
Through Use Of Teams, Nonphysicians, And Electronic Communication. Health
Aff (Millwood). 2013;32(1). Accessed January 21, 2022.
https://doi.org/10.1377/hlthaff.2012.1086
28.Harvard T.H. Chan School of Public Health, Robert Wood Johnson Foundation,
National Public Radio. Patients’ Perspectives on Health Care in the United States:
Texas. Published online 2016.
29.DSRIP Transition | Texas Health and Human Services. Accessed January 20,
2022. https://www.hhs.texas.gov/regulations/policies-rules/waivers/medicaid-
1115-waiver/dsrip-transition
30.Texas Incentives for Physicians and Professional Services (TIPPS) Program |
Texas Health and Human Services. Accessed January 20, 2022.
https://www.hhs.texas.gov/services/health/medicaid-chip/provider-
information/medicaid-chip-directed-payment-programs/texas-incentives-
physicians-professional-services-tipps-program
31.Comprehensive Hospital Increased Reimbursement Program (CHIRP) | Texas
Health and Human Services. Accessed January 20, 2022.
https://www.hhs.texas.gov/services/health/medicaid-chip/provider-
information/medicaid-chip-directed-payment-programs/comprehensive-hospital-
increased-reimbursement-program-chirp
32.Directed Payment Program for Behavioral Health Services (DPP BHS) | Texas
Health and Human Services. Accessed January 20, 2022.
https://www.hhs.texas.gov/services/health/medicaid-chip/provider-
information/medicaid-chip-directed-payment-programs/directed-payment-
program-behavioral-health-services-dpp-bhs
33.Rural Access to Primary and Preventive Services (RAPPS) Program | Texas
Health and Human Services. Accessed January 20, 2022.
https://www.hhs.texas.gov/services/health/medicaid-chip/provider-
67
information/medicaid-chip-directed-payment-programs/rural-access-primary-
preventive-services-rapps-program
34.CDC. What is health literacy? Take action. Find out. Centers for Disease Control
and Prevention. Published February 2, 2022. Accessed September 29, 2022.
https://www.cdc.gov/healthliteracy/learn/index.html
35.Adams RJ. Improving health outcomes with better patient understanding and
education. Risk Manag Healthc Policy. 2010;3:61-72. doi:10.2147/RMHP.S7500
36.Santos P, Sá L, Couto L, Hespanhol A. Health literacy as a key for effective
preventive medicine. Hale R, ed. Cogent Soc Sci. 2017;3(1):1407522.
doi:10.1080/23311886.2017.1407522
37.CDC. The What, Why, and How of Health Literacy. Centers for Disease Control
and Prevention. Published March 29, 2021. Accessed July 7, 2022.
https://www.cdc.gov/healthliteracy/learn/Understanding.html
38.Ranganathan M, Lagarde M. Promoting healthy behaviours and improving health
outcomes in low and middle income countries: A review of the impact of
conditional cash transfer programmes. Prev Med. 2012;55:S95-S105.
doi:10.1016/j.ypmed.2011.11.015
39.U.S. Department of Commerce, U.S. Census Bureau. American Community
Survey: ACS 5-Year Estimates Data Profiles, 2018: Selected Social
Characteristics In The United States. Accessed March 17, 2022.
https://data.census.gov/cedsci/
40.Leider JP, Meit M, McCullough JM, et al. The State of Rural Public Health:
Enduring Needs in a New Decade. Am J Public Health. 2020;110(9):1283-1290.
doi:10.2105/AJPH.2020.305728
41.Hartley D. Rural Health Disparities, Population Health, and Rural Culture. Am J
Public Health. 2004;94(10):1675-1678. doi:10.2105/AJPH.94.10.1675
42.Holmes M. Risk Factors and Potentially Preventable Deaths in Rural
Communities. :4.
43.Johnson JA, Johnson AM. Urban-Rural Differences in Childhood and Adolescent
Obesity in the United States: A Systematic Review and Meta-Analysis. Child
Obes. 2015;11(3):233-241. doi:10.1089/chi.2014.0085
44.Rural Health Information Hub. Rural Health Disparities Introduction.
https://www.ruralhealthinfo.o rg/topics/rural-health-disparities
45.Curtin SC, Spencer MR. Trends in Death Rates in Urban and Rural Areas: United
States, 1999-2019. NCHS Data Brief. 2021;(417):1-8.
46.Bolin JN, Bellamy GR, Ferdinand AO, et al. Rural Healthy People 2020: New
Decade, Same Challenges. J Rural Health. 2015;31(3):326-333.
doi:https://doi.org/10.1111/jrh.12116
68
47.Texas Department of State Health Services. Office of Border Health. Accessed
February 26, 2021. https://www.dshs.texas.gov/borderhealth/
48.Texas Attorney General. Colonias Terms. Accessed February 26, 2021.
https://www.texasattorneygeneral.gov/divisions/colonias-prevention/colonias-
terms
49.Mier N, Ory MG, Zhan D, Conkling M, Sharkey JR, Burdine JN. Health-related
quality of life among Mexican Americans living in colonias at the Texas–Mexico
border. Soc Sci Med. 2008;66(8):1760-1771.
doi:10.1016/j.socscimed.2007.12.017
50.Ullrich F, Mueller K. COVID-19 Cases and Deaths, Metropolitan and
Nonmetropolitan Counties Over Time (update). RUPRI Cent Rural Health Policy
Anal Rural Data Brief. 2022;2020-9. https://rupri.public-
health.uiowa.edu/publications/policybriefs/2020/COVID%20Longitudinal%20Dat
a.pdf
51.Lakhani HV, Pillai SS, Zehra M, Sharma I, Sodhi K. Systematic Review of Clinical
Insights into Novel Coronavirus (CoVID-19) Pandemic: Persisting Challenges in
U.S. Rural Population. Int J Environ Res Public Health. 2020;17(12):E4279.
doi:10.3390/ijerph17124279
52.CDC. Coronavirus Disease 2019 (COVID-19). Centers for Disease Control and
Prevention. Published February 11, 2020. Accessed March 30, 2022.
https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/underlying-
evidence-table.html
53.Sun Y, Monnat SM. Rural-urban and within-rural differences in COVID-19
vaccination rates. J Rural Health Off J Am Rural Health Assoc Natl Rural Health
Care Assoc. Published online September 23, 2021. doi:10.1111/jrh.12625
54.Sociodemographic Determinants of COVID-19 Vaccine Hesitancy, Fear of
Infection, and Protection Self-Efficacy - PMC. Accessed March 29, 2022.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8388227/
55.Texas Department of Agriculture, Texas Rural Health and Economic Advisory
Council. 2018 Rural Policy Plan Report.; 2018.
https://www.texasagriculture.gov/Portals/0/Publications/ER/2018%20Rural%20
Policy%20Plan%20Report.pdf
56.Rural Emergency Medical Services (EMS) and Trauma Overview - Rural Health
Information Hub. Accessed September 29, 2022.
https://www.ruralhealthinfo.org/topics/emergency-medical-services#workforce
57.Texas EMS Alliance. The Issues – 1. Accessed February 26, 2021.
http://txemsa.com/the-issues/
58.87(3) SB 8 - Enrolled version - Bill Text. Accessed September 29, 2022.
https://capitol.texas.gov/tlodocs/873/billtext/html/SB00008F.htm
69
59.Scholarships for EMS Education and Training Available from DSHS. Accessed
September 29, 2022. https://www.dshs.texas.gov/news-alerts/scholarships-
ems-education-training-available-dshs/
60.Centers for Medicaid and Medicare Services. President Trump Expands
Telehealth Benefits for Medicare Beneficiaries During COVID-19 Outbreak.
Published May 17, 2020. https://www.cms.gov/newsroom/press-
releases/president-trump-expands-telehealth-benefits-medicare-beneficiaries-
during-covid-19-outbreak
61.Office of the Texas Governor. Governor Abbott Waives Regulations, Expands
Telehealth Options. Published April 9, 2020.
https://gov.texas.gov/news/post/governor-abbott-waives-regulations-expands-
telehealth-options
62.Texas A&M University Rural and Community Health Institute. What’s Next?
Practical Suggestions for Rural Communities Facing a Hospital Closure.; 2017.
https://architexas.org/news/whats-next-final-rchi.pdf
63.Mulverhill. Texas’ Digital Divide. Texas Comptroller of Public. Accessed February
26, 2021. https://comptroller.texas.gov/economy/fiscal-
notes/2019/oct/divide.php
64.Rural Health Research Gateway. Rural Health Research Recap: Rural
Communities: Age, Income, and Health Status.; 2018.
https://www.ruralhealthresearch.org/assets/2200-8536/rural-communities-age-
income-health-status-recap.pdf
65.Texas Demographic Center. 2018 Estimated Population of Texas, Its Counties,
and Places.; 2019.
https://demographics.texas.gov/Resources/publications/2019/20191205_PopEst
imatesBrief.pdf
66.Office of Disease Prevention and Health Promotion. 2020 Topics & Objectives:
Older Adults. healthypeople.gov. https://www.healthypeople.gov/2020/topics-
objectives/topic/older-adults
67.US Census Bureau. Uninsured Rate by State: 2008 to 2018. The United States
Census Bureau. Accessed January 22, 2021.
https://www.census.gov/library/visualizations/interactive/uninsured-rate-2008-
2018.html
68.Khullar D, Chokshi D. Health, Income, & Poverty: Where We Are & What Could
Help, Health Affairs Briefs. Published online October 4, 2018.
doi:10.1377/hpb20180817.901935
69.Texas Organization of Rural and Community Hospitals. Rural Hospital Closures.
torchnet.org. Accessed January 14, 2021. https://www.torchnet.org/advocacy--
rural-hospital-closure.html
70
70.Wishner J, Solleveld P, Rudowitz R, Paradise J, Antonisse L. A Look at Rural
Hospital Closures and Implications for Access to Care: Three Case Studies. The
Urban Institute and Kaiser Family Foundation; 2016.
http://www.urban.org/sites/default/files/publication/82511/2000857-brief-a-
look-at-rural-hospital-closures-and-implications-for-access-to-care.pdf
71.Hsia RYJ, Shen YC. Rising Closures Of Hospital Trauma Centers
Disproportionately Burden Vulnerable Populations. Health Aff (Millwood).
2011;30(10):1912-1920. doi:10.1377/hlthaff.2011.0510
72.Flinn B. Nursing Home Closures and Trends June 2015 - June 2019. Leading
Age. Published February 2020.
https://leadingage.org/sites/default/files/Nursing%20Home%20Closures%20an
d%20Trends%202020.pdf
73.Garfield R, Orgera K, Damico A. The Coverage Gap: Uninsured Poor Adults in
States That Do Not Expand Medicaid. Kaiser Family Foundation; 2020.
https://www.kff.org/medicaid/issue-brief/the-coverage-gap-uninsured-poor-
adults-in-states-that-do-not-expand-medicaid/
75.Artiga S, Damico A, Garfield R. The Impact of the Coverage Gap for Adults in
States Not Expanding Medicaid by Race and Ethnicity. Kaiser Family Foundation;
2015. https://www.kff.org/racial-equity-and-health-policy/issue-brief/the-
impact-of-the-coverage-gap-in-states-not-expanding-medicaid-by-race-and-
ethnicity/
76.Lindrooth RC, Perraillon MC, Hardy RY, Tung GJ. Understanding The Relationship
Between Medicaid Expansions And Hospital Closures. Health Aff (Millwood).
2018;37(1):111-120. doi:10.1377/hlthaff.2017.0976
77.Collins C, Novack S. Critical Condition: Part 2: Driving My Life Away. Tex Obs.
Published online November 18, 2019. Accessed January 15, 2021.
https://www.texasobserver.org/driving-my-life-away/
78.Hernandez R. The Rural Health Care Crisis,
Mapped.https://www.texasobserver.org/the-rural-health-care-crisis-mapped/.
Published November 20, 2019. Accessed January 22, 2021.
79.Texas Department of State Health Services. Texas Physician Supply and
Demand Projections, 2018 - 2032.; 2020.
80.Hung P, Kozhimannil KB, Casey MM, Moscovice IS. Why Are Obstetric Units in
Rural Hospitals Closing Their Doors? Health Serv Res. 2016;51(4):1546-1560.
doi:10.1111/1475-6773.12441
81.Kozhimannil KB, Hung P, Henning-Smith C, Casey MM, Prasad S. Association
Between Loss of Hospital-Based Obstetric Services and Birth Outcomes in Rural
Counties in the United States. JAMA. 2018;319(12):1239-1247.
doi:10.1001/jama.2018.1830
71
82.Pennsylvania Rural Health Model. Pennsylvania Department of Health. Accessed
March 30, 2022. https://www.health.pa.gov:443/topics/Health-
Innovation/Pages/Rural-Health.aspx
83.A&M Rural and Community Health Institute. Accessed March 29, 2022.
https://www.architexas.org/
84.Health Resources and Services Administration. A Guide for Rural Health Care
Collaboration and Coordination. Published online August 2019.
https://www.hrsa.gov/sites/default/files/hrsa/ruralhealth/reports/HRSA-Rural-
Collaboration-Guide.pdf
85.U.S. Department of Commerce, U.S. Census Bureau. American Community
Survey: ACS 1-Year Estimates Subject Tables, 2019: Selected Characteristics Of
Health Insurance Coverage In The United States. Accessed March 30, 2022.
https://data.census.gov/cedsci/table?q=United%20States&t=Health%20Insuran
ce&g=0400000US48
86.Families USA, National Center for Coverage Innovation. The COVID-19 Pandemic
and Resulting Economic Crash Have Caused the Greatest Health Insurance
Losses in American History. Accessed March 30, 2022. https://fam
iliesusa.org/wp-content/uploads/2020/07/COV-254_Coverage-Loss_Report_7-
17-20.pdf
87.Hear Us Out Campaign Reports Nurses’ COVID-19 Reality - AACN. Accessed
March 29, 2022. https://www.aacn.org/newsroom/hear-us-out-campaign-
reports-nurses-covid-19-reality
88.Alrawashdeh HM, Al-Tammemi AB, Alzawahreh MKh, et al. Occupational burnout
and job satisfaction among physicians in times of COVID-19 crisis: a convergent
parallel mixed-method study. BMC Public Health. 2021;21(1):811.
doi:10.1186/s12889-021-10897-4
89.Bureau of Labor Statistics. The Employment Situation - February 2022.
Published online March 2022. https://www.bls.gov/news.release/pdf/empsit.pdf
90.Rural Texans hit hardest as state sees shortage of primary care doctors during
the pandemic. KUT Radio, Austin’s NPR Station. Published November 18, 2021.
Accessed July 7, 2022. https://www.kut.org/health/2021-11-18/rural-texans-
hit-hardest-as-state-sees-shortage-of-primary-care-doctors-during-the-
pandemic
91.‘Nursing Is in Crisis’: Staff Shortages Put Patients at Risk. N Y Times. Published
online August 21, 2021.
https://www.pnns.org/resources/Documents/Jacobs%20NYT%20August%20202
1%20_Nursing%20Is%20in%20Crisis%E2%80%99_%20Staff%20Shortages%2
0Put%20Patients%20at%20Risk%20-%20The%20New%20York%20Times.pdf
72
92.Texas Higher Education Coordinating Board. Types of Financial Aid - Loan
Repayment Programs. Accessed March 30, 2022.
http://www.hhloans.com/apps/financialaid/tofa.cfm?Kind=LRP
93.Report on Residents. AAMC. Accessed March 29, 2022.
https://www.aamc.org/data-reports/students-residents/report/report-residents
94.Health Resources and Services Administration. 2016 NHSC Participant
Satisfaction Survey Results. Published online January 2017.
https://www.hrsa.gov/sites/default/files/hrsa/advisory-committees/national-
health-service-corps/advisory-council-meeting-January-2017-nhsc-participant-
survey-results.pdf
95.Lam O, Broderick B, Toor S. How far Americans live from the closest hospital
differs by community type. Pew Research Center. Accessed March 24, 2022.
https://www.pewresearch.org/fact-tank/2018/12/12/how-far-americans-live-
from-the-closest-hospital-differs-by-community-type/
96.The Caring Foundation of Texas. Care Van. Caring Foundation of Texas.
Accessed March 30, 2022. https://carevan.org/
97.Texas Broadband Development Office. Accessed April 26, 2022.
https://comptroller.texas.gov/programs/broadband/legislation.php
98.Walker JH, Dewitt DE, Pallant JF, Cunningham CE. Rural origin plus a rural
clinical school placement is a significant predictor of medical students’ intentions
to practice rurally: a multi-university study. Rural Remote Health.
2012;12:1908.
99.Health Professions Recruitment and Exposure Program (HPREP): Non-degree
Programs - UT Southwestern, Dallas, TX. Accessed April 4, 2022.
https://www.utsouthwestern.edu/education/programs/nondegree-
programs/high-school-students/hprep/
100. Texas Center for Nursing Workforce Studies. 2021 Nursing Education for High
School Students. Published online March 2022.
https://dshs.texas.gov/chs/cnws/NEPIS/2021/2021_NEPIS_HighSchool.pdf
101. Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime
Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National
Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593-602.
doi:10.1001/archpsyc.62.6.593
102. The Hogg Foundation for Mental Health and Methodist Healthcare Ministries.
Crisis Point: Mental Health Workforce Shortages in Texas. Accessed May 4,
2022. https://www.mhm.org/library/policy-publications/crisis-point-mental-
health-workforce-shortages-in-texas/
103. National Research Council (US) and Institute of Medicine (US) Committee on
the Prevention of Mental Disorders and Substance Abuse Among Children,
73
Youth, and Young Adults: Research Advances and Promising Interventions.
Preventing Mental, Emotional, and Behavioral Disorders Among Young People:
Progress and Possibilities. (O’Connell ME, Boat T, Warner KE, eds.). National
Academies Press (US); 2009. Accessed May 4, 2022.
http://www.ncbi.nlm.nih.gov/books/NBK32775/
104. U.S Department of Health and Human Services, Substance Abuse and Mental
Health Services Administration, Center for Behavioral Health Statistics and
Quality, Populations Survey Branch. Key Substance Use and Mental Health
Indicators in the United States: Results from the 2020 National Survey on Drug
Use and Health. Published online 2020:156.
105. Cunningham PJ. Beyond Parity: Primary Care Physicians’ Perspectives On
Access To Mental Health Care. Health Aff (Millwood). 2009;28(Supplement
1):w490-w501. doi:10.1377/hlthaff.28.3.w490
106. Burea of Health Workforce, Health Resources and Services Administration
(HRSA), U.S. Department of Health & Human Services. Designated Health
Professional Shortage Areas Statistics: Second Quarter of Fiscal Year 2022.
Published online March 31, 2022.
https://data.hrsa.gov/Default/GenerateHPSAQuarterlyReport
107. American Psychological Association. Psychology and aging: Addressing
mental health needs of older adults: (526182009-001). Published online 2009.
doi:10.1037/e526182009-001
108. Hoge MA, Stuart GW, Morris J, Flaherty MT, Paris M, Goplerud E. Mental
Health And Addiction Workforce Development: Federal Leadership Is Needed To
Address The Growing Crisis. Health Aff (Millwood). 2013;32(11):2005-2012.
doi:10.1377/hlthaff.2013.0541
109. U.S. Department of Health and Human Services, Health Resources and
Services Administration, National Center for Health Workforce Analysis.
Behavioral Health Workforce Projections: Addiction Counselors. Accessed May 4,
2022. https://bhw.hrsa.gov/data-research/projecting-health-workforce-supply-
demand/behavioral-health
110. Thomas KC, Ellis AR, Konrad TR, Holzer CE, Morrissey JP. County-Level
Estimates of Mental Health Professional Shortage in the United States. Psychiatr
Serv. 2009;60(10):1323-1328. doi:10.1176/ps.2009.60.10.1323
111. Texas Health and Human Services Commission, Behavioral Health Services
Section, Office of Decision Support. Data Provided August 8, 2018.
112. Texas Department of State Health Services. Youth Risk Behavior Survey
(YRBS), 2019. Accessed May 4, 2022.
https://healthdata.dshs.texas.gov/dashboard/surveys-and-profiles/yrbs
74
113. Tomblin Murphy G, Birch S, MacKenzie A, Alder R, Lethbridge L, Little L.
Eliminating the shortage of registered nurses in Canada: An exercise in applied
needs-based planning. Health Policy. 2012;105(2):192-202.
doi:10.1016/j.healthpol.2011.11.009
114. Texas Department of State Health Services, Texas Primary Care Office. Data
Provided June 16, 2020.
115. Thomas KC, Ellis AR, Konrad TR, Morrissey JP. North Carolina’s mental health
workforce: unmet need, maldistribution, and no quick fixes. N C Med J.
2012;73(3):161-168.
116. Texas Department of State Health Services, Texas Health & Human Services.
Texas Physician Supply and Demand Projections, 2018 - 2032. Published online
May 2020. https://dshs.texas.gov/legislative/2020-
Reports/TexasPhysicianSupplyDemandProjections-2018-2032.pdf
117. Texas Health Professions Resource Center Mental Health Professions 2021
Data.
118. American School Counselor Association. Student-to-School-Counselor Ratio
2020–2021. https://www.schoolcounselor.org/getmedia/238f136e-ec52-4bf2-
94b6-f24c39447022/Ratios-20-21-Alpha.pdf
119. National Association of School Psychologists. NASP Policy Platform. National
Association of School Psychologists (NASP). Accessed May 4, 2022.
https://www.nasponline.org/research-and-policy/policy-priorities/nasp-policy-
platform
120. Texas Education Agency, PEIMS Reporting Unit, Research and Analysis
Division. Staff FTE Counts and Salary Reports. Accessed May 4, 2022.
https://rptsvr1.tea.texas.gov/adhocrpt/adpeb.html
121. Texas Education Agency, Office of Governance and Accountability, Division of
Research and Analysis. Enrollment in Texas Public Schools 2020-21. Published
online 2021:86.
122. The Mayo Clinic Health System. College Students and Depression. Mayo
Clinic Health System. Accessed June 27, 2022.
https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-
health/college-students-and-depression
123. Son C, Hegde S, Smith A, Wang X, Sasangohar F. Effects of COVID-19 on
College Students’ Mental Health in the United States: Interview Survey Study. J
Med Internet Res. 2020;22(9):e21279. doi:10.2196/21279
124. Centers for Disease Control and Prevention. Youth Online: High School YRBS
- Texas 2019 Results. Accessed May 4, 2022.
https://nccd.cdc.gov/youthonline/app/Results.aspx?TT=A&OUT=0&SID=HS&QI
D=QQ&LID=TX&YID=2019&LID2=&YID2=&COL=S&ROW1=N&ROW2=N&HT=Q
75
Q&LCT=LL&FS=S1&FR=R1&FG=G1&FA=A1&FI=I1&FP=P1&FSL=S1&FRL=R1&F
GL=G1&FAL=A1&FIL=I1&FPL=P1&PV=&TST=False&C1=&C2=&QP=G&DP=1&VA
=CI&CS=Y&SYID=&EYID=&SC=DEFAULT&SO=ASC
125. Texas Legislature Online. 86(R) History for SB 11. Accessed May 4, 2022.
https://capitol.texas.gov/BillLookup/History.aspx?LegSess=86R&Bill=SB11
126. Texas Health and Safety Code, Section 113.0052. Accessed May 4, 2022.
https://statutes.capitol.texas.gov/Docs/HS/htm/HS.113.htm
127. The University of Texas System. TCMHCC – Texas Child Mental Health Care
Consortium. Accessed May 4, 2022. https://tcmhcc.utsystem.edu/
128. Texas Health and Safety Code, Section 113.0101. Accessed May 4, 2022.
https://statutes.capitol.texas.gov/Docs/HS/htm/HS.113.htm
129. Texas Health and Safety Code, Section 113.0051. Accessed May 4, 2022.
https://statutes.capitol.texas.gov/Docs/HS/htm/HS.113.htm
130. Texas Health and Safety Code, Sections 113.0201 and 113.0202. Accessed
May 4, 2022. https://statutes.capitol.texas.gov/Docs/HS/htm/HS.113.htm
131. Texas Legislature Online. 87(R) History for SB 1. Accessed May 4, 2022.
https://capitol.texas.gov/billlookup/History.aspx?LegSess=87R&Bill=SB1
132. General Appropriations Act for the 2016-17 Biennium, Eighty-fourth Texas
Legislature, Regular Session, 2015.
https://capitol.texas.gov/tlodocs/87R/billtext/pdf/SB00001F.pdf
133. Texas Government Code, Section 531.472.
https://statutes.capitol.texas.gov/Docs/GV/htm/GV.531.htm
134. 87(R) HB 4074 - Senate Committee Report version - Bill Text. Accessed May
4, 2022. https://capitol.texas.gov/tlodocs/87R/billtext/html/HB04074S.htm
135. Texas Statewide Behavioral Health Coordinating Council. Texas Statewide
Behavioral Health Strategic Plan, Fiscal Years 2017-2021.; 2016.
http://mmhpi.org/wp-content/uploads/2018/07/Statewide-Behavioral-Health-
Strategic-Plan.pdf
136. Texas Administrative Code, Title 19, Part 1, Chapter 23, Subchapter D.
https://texreg.sos.state.tx.us/public/readtac$ext.ViewTAC?tac_view=5&ti=19&p
t=1&ch=23&sch=D&rl=Y
137. Texas Administrative Code, Title 19, Part 1, Chapter 23, Subchapter D, Rule
§23.95.
https://texreg.sos.state.tx.us/public/readtac$ext.TacPage?sl=R&app=9&p_dir=
&p_rloc=&p_tloc=&p_ploc=&pg=1&p_tac=&ti=19&pt=1&ch=23&rl=95
138. Texas Administrative Code, Title 19, Part 1, Chapter 23, Subchapter D, Rule
§23.96.
https://texreg.sos.state.tx.us/public/readtac$ext.TacPage?sl=R&app=9&p_dir=
&p_rloc=&p_tloc=&p_ploc=&pg=1&p_tac=&ti=19&pt=1&ch=23&rl=96
76
139. St. John Fisher College. Federal Grant Expands Mental Health Program.
Published 2021. Accessed May 4, 2022. https://www.sjfc.edu/news-and-
events/news-archive/fall-2021/federal-grant-expands-mental-health-program/
140. Center for Disease Control and Prevention. Mental Health - Household Pulse
Survey - COVID-19. Published April 20, 2022. Accessed May 4, 2022.
https://www.cdc.gov/nchs/covid19/pulse/mental-health.htm
141. Texas Department of State Health Services. HHSC Launches $23.2 Million
Substance Use Prevention Awareness Campaign Effort | Texas Health and
Human Services. Accessed May 4, 2022.
https://www.hhs.texas.gov/news/2022/03/hhsc-launches-23-2-million-
substance-use-prevention-awareness-campaign-effort
142. Centers for Disease Control and Prevention, National Center for Health
Statistics. Provisional Drug Overdose Data. Published April 5, 2022. Accessed
May 4, 2022. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
143. Texas Health and Human Services. COVID-19 Mental Health Support Line
Helps Thousands of Texans. Accessed May 4, 2022.
https://www.hhs.texas.gov/news/2021/09/covid-19-mental-health-support-line-
helps-thousands-texans
144. Statewide Behavioral Health Coordinating Council. Strong Families,
Supportive Communities: Moving Our Behavioral Health Workforce Forward.;
2020. Accessed May 4, 2020.
https://www.hhs.texas.gov/sites/default/files/documents/laws-
regulations/reports-presentations/2020/behavioral-health-workforce-workgroup-
report-dec-2020.pdf
145. Health Resources & Services Administration. Shortage Areas. Accessed May
16, 2022. https://data.hrsa.gov/topics/health-workforce/shortage-areas
146. Texas Health and Human Services. Texas HHS Receives National Suicide
Prevention Lifeline Grant | Texas Health and Human Services. Published 2021.
Accessed May 4, 2022. https://www.hhs.texas.gov/news/2021/02/texas-hhs-
receives-national-suicide-prevention-lifeline-grant
147. Telemedicine | Medicaid. Medicaid.gov. Accessed February 22, 2022.
https://www.medicaid.gov/medicaid/benefits/telemedicine/index.html
148. OCCUPATIONS CODE CHAPTER 111. TELEMEDICINE, TELEDENTISTRY, AND
TELEHEALTH. Accessed February 22, 2022.
https://statutes.capitol.texas.gov/Docs/OC/htm/OC.111.htm
149. Achenbach SJ. Telemedicine: Benefits, Challenges, and its Great Potential.
Health Law Policy Brief. 2020;14(1):26.
150. 2000, Program Authorization, Services and Definitions. Accessed February
22, 2022. https://www.hhs.texas.gov/book/export/html/266896
77
151. Texas Health and Human Services. Telemedicine, Telehealth, and Home
Telemonitoring Services in Texas Medicaid. Accessed November 17, 2021.
https://www.hhs.texas.gov/sites/default/files/documents/laws-
regulations/reports-presentations/2020/sb-789-telemedicine-telehealth-hts-
medicaid-dec-2020.pdf
152. E-Health Advisory Committee | Texas Health and Human Services. Accessed
October 27, 2021. https://www.hhs.texas.gov/about/leadership/advisory-
committees/e-health-advisory-committee
153. Public Health Emergency. U.S. Department of Health & Human Services.
Accessed October 27, 2021.
https://www.phe.gov/emergency/news/healthactions/phe/Pages/default.aspx
154. Governor Abbott Waives Certain Regulations For Telemedicine Care In
Texas.https://gov.texas.gov/news/post/governor-abbott-waives-certain-
regulations-for-telemedicine-care-in-texas. Published March 17, 2020. Accessed
November 17, 2021.
155. Governor Abbott Announces Agreement With Health Insurers To Continue
Payment Parity For Telehealth. Published September 25, 2020. Accessed
November 17, 2021. https://gov.texas.gov/news/post/governor-abbott-
announces-agreement-with-health-insurers-to-continue-payment-parity-for-
telehealth
156. Texas HB4 | 2021-2022 | 87th Legislature. LegiScan. Accessed November
22, 2021. https://legiscan.com/TX/text/HB4/id/2407389
157. Texas SB228 | 2021-2022 | 87th Legislature. LegiScan. Accessed November
17, 2021. https://legiscan.com/TX/text/SB228/id/2218519
158. Texas SB434 | 2021-2022 | 87th Legislature. LegiScan. Accessed November
17, 2021. https://legiscan.com/TX/bill/SB434/2021
159. Texas SB488 | 2021-2022 | 87th Legislature. LegiScan. Accessed January
16, 2021. https://legiscan.com/TX/drafts/SB488/2021
160. Texas Health and Human Services. Assessment of Texas Medicaid Rural
Teleservices.; :96. Accessed November 17, 2021.
https://www.hhs.texas.gov/sites/default/files/documents/laws-
regulations/policies-rules/Waivers/medicaid-1115-waiver/assessment-texas-
medicaid-rural-teleservices.pdf
161. Texas Medicaid & CHIP Teleservices Monthly Trend | Texas Health and
Human Services. Accessed January 12, 2022.
https://www.hhs.texas.gov/data/texas-medicaid-chip-teleservices-monthly-
trend
78
162. Mosquera RA, Avritscher EBC, Pedroza C, et al. Telemedicine for Children
With Medical Complexity: A Randomized Clinical Trial. Pediatrics.
2021;148(3):e2021050400. doi:10.1542/peds.2021-050400
163. Ramirez AV, Ojeaga M, Espinoza V, Hensler B, Honrubia V. Telemedicine in
Minority and Socioeconomically Disadvantaged Communities Amidst COVID-19
Pandemic. Otolaryngol Neck Surg. 2021;164(1):91-92.
doi:10.1177/0194599820947667
164. Texas Launches Broadband Office to Guide Expansion. GovTech. Published
August 6, 2021. Accessed November 3, 2021.
https://www.govtech.com/civic/texas-launches-broadband-office-to-guide-
expansion
165. Texas Legislature Online - 87(3) History for HB 76. Accessed November 3,
2021.
https://capitol.texas.gov/BillLookup/History.aspx?LegSess=873&Bill=HB76
166. mHealthIntelligence. Texas Lawmaker Eyes Telehealth Program for Rural 911
Services. mHealthIntelligence. Published October 13, 2021. Accessed November
3, 2021. https://mhealthintelligence.com/news/texas-lawmaker-eyes-
telehealth-program-for-rural-911-services
167. Telemedicine Policy, Regulations, and Reimbursement in Texas. Accessed
November 3, 2022. https://www.texmed.org/telemedicine/
168. Physician License. Interstate Medical Licensure Compact. Accessed December
10, 2022. https://www.imlcc.org/
169. Weiner S. What happens to telemedicine after COVID-19? AAMC.
https://www.aamc.org/news-insights/what-happens-telemedicine-after-covid-
19. Published October 21, 2021. Accessed November 11, 2021.
170. Medicaid and CHIP Teleservices | Texas Health and Human Services.
Accessed December 15, 2021.
https://www.hhs.texas.gov/services/health/medicaid-chip/provider-
information/medicaid-chip-teleservices
171. HIE Benefits | HealthIT.gov. The Office of the National Coordinator for Health
Information Technology (ONC). Published October 12, 2017. Accessed April 6,
2022. https://www.healthit.gov/topic/health-it-and-health-information-
exchange-basics/hie-benefits
172. HITECH Act Enforcement Interim Final Rule. HHS.gov. Published October 28,
2009. Accessed April 6, 2022. https://www.hhs.gov/hipaa/for-
professionals/special-topics/hitech-act-enforcement-interim-final-rule/index.html
173. Statewide Health Information Exchange | Texas Health and Human Services.
Texas Health and Human Services. Accessed April 6, 2022.
https://www.hhs.texas.gov/about/process-improvement/improving-services-
79
texans/health-informatics-services-quality/statewide-health-information-
exchange
174. Nachum S, Gogia K, Clark S, Hsu H, Sharma R, Greenwald PW. An Evaluation
of Kiosks for Direct-to-Consumer Telemedicine Using the National Quality Forum
Assessment Framework. Telemed E-Health. 2021;27(2):178-183.
doi:10.1089/tmj.2019.0318
